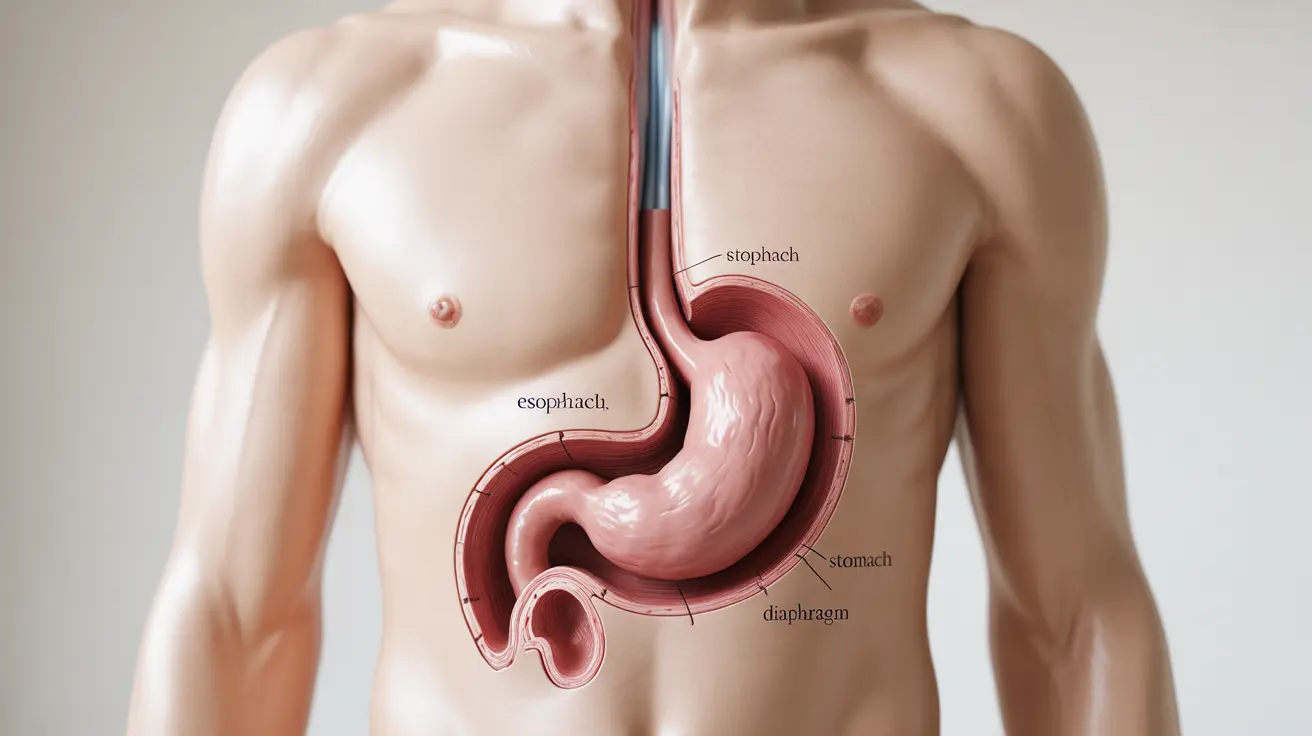
A hiatal hernia occurs when part of the stomach pushes through the diaphragm, the muscle that separates the chest cavity from the abdomen. This common condition can affect people of all ages, though it's more prevalent in older adults and those with certain risk factors. Understanding its symptoms, causes, and treatment options is crucial for managing this condition effectively.
While many people with hiatal hernias may not experience symptoms, others can face significant discomfort that affects their daily life. This comprehensive guide will help you understand the condition better and explore various management strategies.
What is a Hiatal Hernia?
A hiatal hernia develops when a portion of the stomach protrudes through the hiatus, a natural opening in the diaphragm that allows the esophagus to connect to the stomach. This condition can vary in severity and size, ranging from small hernias that cause minimal issues to larger ones that may require medical intervention.
Types of Hiatal Hernias
Sliding Hiatal Hernia
This most common type occurs when the stomach and the section of the esophagus that joins the stomach slide up into the chest through the hiatus. These hernias typically move in and out of the chest cavity.
Paraesophageal Hernia
This less common but more serious type occurs when part of the stomach pushes through the hiatus and remains next to the esophagus. These hernias require closer monitoring due to potential complications.
Common Symptoms and Warning Signs
Many people with hiatal hernias may experience:
- Heartburn and acid reflux
- Chest pain or pressure
- Difficulty swallowing
- Regurgitation of food or liquids
- Shortness of breath after eating
- Feeling uncomfortably full after meals
Risk Factors and Causes
Several factors can increase your risk of developing a hiatal hernia:
- Age (more common in people over 50)
- Obesity
- Pregnancy
- Frequent heavy lifting
- Chronic coughing or straining
- Genetic predisposition
Diagnosis Methods
Healthcare providers typically use several diagnostic tools to confirm a hiatal hernia:
- Barium X-ray studies
- Upper endoscopy
- CT scans
- MRI imaging
- pH monitoring tests
Treatment Approaches
Lifestyle Modifications
Initial treatment often focuses on lifestyle changes:
- Maintaining a healthy weight
- Eating smaller meals
- Avoiding lying down after meals
- Elevating the head of the bed
- Avoiding trigger foods
Medications
Various medications may help manage symptoms:
- Antacids for quick acid relief
- H2 blockers to reduce acid production
- Proton pump inhibitors (PPIs) for long-term acid control
Surgical Options
Surgery might be recommended when other treatments aren't effective or in cases of severe hernias. Common procedures include laparoscopic repair and fundoplication.
Frequently Asked Questions
- What are the common symptoms of a hiatal hernia and how can I recognize them?
Common symptoms include heartburn, chest pain, difficulty swallowing, and regurgitation of food. You might also experience shortness of breath after eating and feel unusually full after meals. However, some people may have no symptoms at all.
- What causes a hiatal hernia and who is most at risk for developing one?
Hiatal hernias can be caused by increased pressure in the abdominal cavity, weakened muscle tissue, or injury. People over 50, those who are overweight, pregnant women, and individuals who frequently lift heavy objects are at higher risk.
- How is a hiatal hernia diagnosed and what tests are typically used?
Diagnosis usually involves imaging tests such as barium X-rays, upper endoscopy, CT scans, or MRI. Your doctor will choose the most appropriate test based on your symptoms and medical history.
- What treatment options, including lifestyle changes and medications, are available for managing hiatal hernia symptoms?
Treatment options range from lifestyle changes (like weight management and dietary modifications) to medications (such as antacids and PPIs). The approach depends on symptom severity and individual patient factors.
- When is surgery recommended for a hiatal hernia, and what types of surgical procedures are commonly performed?
Surgery is typically recommended for large hernias, severe symptoms that don't respond to other treatments, or complications like strangulation. Common procedures include laparoscopic hernia repair and Nissen fundoplication, which can often be performed minimally invasively.