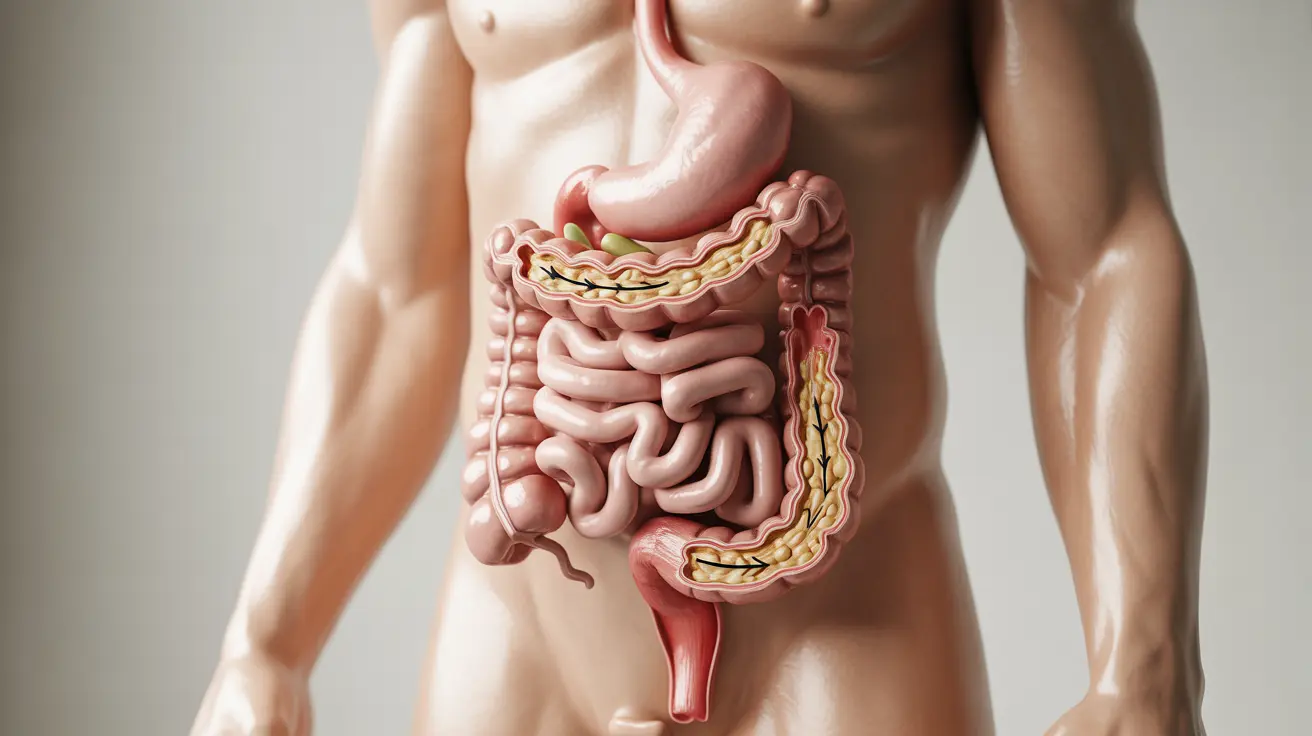
Ileus is a serious condition where the normal movement of the intestines slows down or stops completely, leading to a buildup of food, fluid, and gas in the digestive system. This condition commonly occurs after abdominal surgery but can also develop due to various other medical conditions. Understanding ileus is crucial for recognizing its symptoms early and seeking appropriate medical attention.
While temporary slowing of intestinal function is normal after surgery, prolonged ileus can lead to complications and extended hospital stays. This comprehensive guide explores the causes, symptoms, diagnosis, and treatment options for ileus, helping you better understand this challenging condition.
Common Causes and Risk Factors
Several factors can contribute to the development of ileus:
- Abdominal or pelvic surgery
- Infections and inflammation
- Certain medications (especially opioid pain relievers)
- Electrolyte imbalances
- Neurological conditions
Risk factors that may increase the likelihood of developing ileus include:
- Advanced age
- History of abdominal surgeries
- Chronic medical conditions
- Extended bed rest
- Poor physical condition before surgery
Recognizing the Symptoms
Early recognition of ileus symptoms is essential for prompt treatment. Common signs include:
- Abdominal distention or bloating
- Nausea and vomiting
- Absence of bowel movements or gas
- Abdominal pain or cramping
- Loss of appetite
- Difficulty breathing due to pressure on the diaphragm
Diagnostic Procedures
Healthcare providers use various methods to diagnose ileus:
Physical Examination
Doctors will check for abdominal distention, listen for bowel sounds, and assess pain levels.
Imaging Tests
Several imaging techniques may be used:
- X-rays to visualize intestinal obstruction
- CT scans for detailed views of the abdomen
- Ultrasound in certain cases
Laboratory Tests
Blood tests help identify:
- Electrolyte imbalances
- Signs of infection
- Other underlying conditions
Treatment Approaches
Treatment for ileus focuses on supporting bowel function recovery and addressing underlying causes:
Conservative Management
- Temporarily stopping oral intake
- Nasogastric tube placement
- IV fluids and electrolyte correction
- Early mobilization when possible
Medical Interventions
Doctors may prescribe:
- Medications to stimulate bowel movement
- Pain management alternatives to opioids
- Treatment for underlying conditions
Prevention and Recovery
Several strategies can help prevent ileus or support recovery:
- Early mobilization after surgery
- Proper pain management
- Balanced nutrition
- Regular physical activity when appropriate
- Following medical team recommendations
Frequently Asked Questions
What causes ileus and which factors increase the risk of developing it?
Ileus commonly occurs after abdominal surgery, but can also be caused by infections, medications (particularly opioids), electrolyte imbalances, and neurological conditions. Risk factors include advanced age, previous abdominal surgeries, and extended periods of inactivity.
What are the common symptoms of ileus that I should watch for after surgery?
Key symptoms include abdominal bloating, nausea, vomiting, absence of bowel movements or gas, abdominal pain, and decreased appetite. If you experience these symptoms after surgery, notify your healthcare provider immediately.
How is ileus diagnosed and what tests are used to confirm it?
Diagnosis typically involves physical examination, listening for bowel sounds, and imaging tests such as X-rays or CT scans. Blood tests may also be performed to check for underlying conditions and electrolyte imbalances.
What treatments are available to relieve ileus and restore normal bowel movement?
Treatment options include bowel rest, nasogastric tube decompression, IV fluids, and medications to stimulate bowel movement. Early mobilization and addressing underlying causes are also crucial components of treatment.
Can ileus be prevented after abdominal surgery, and what self-care measures help recovery?
While not always preventable, early mobilization, proper pain management, and following post-surgical instructions can help reduce the risk. During recovery, maintaining good nutrition, staying active as allowed, and following medical advice are essential self-care measures.