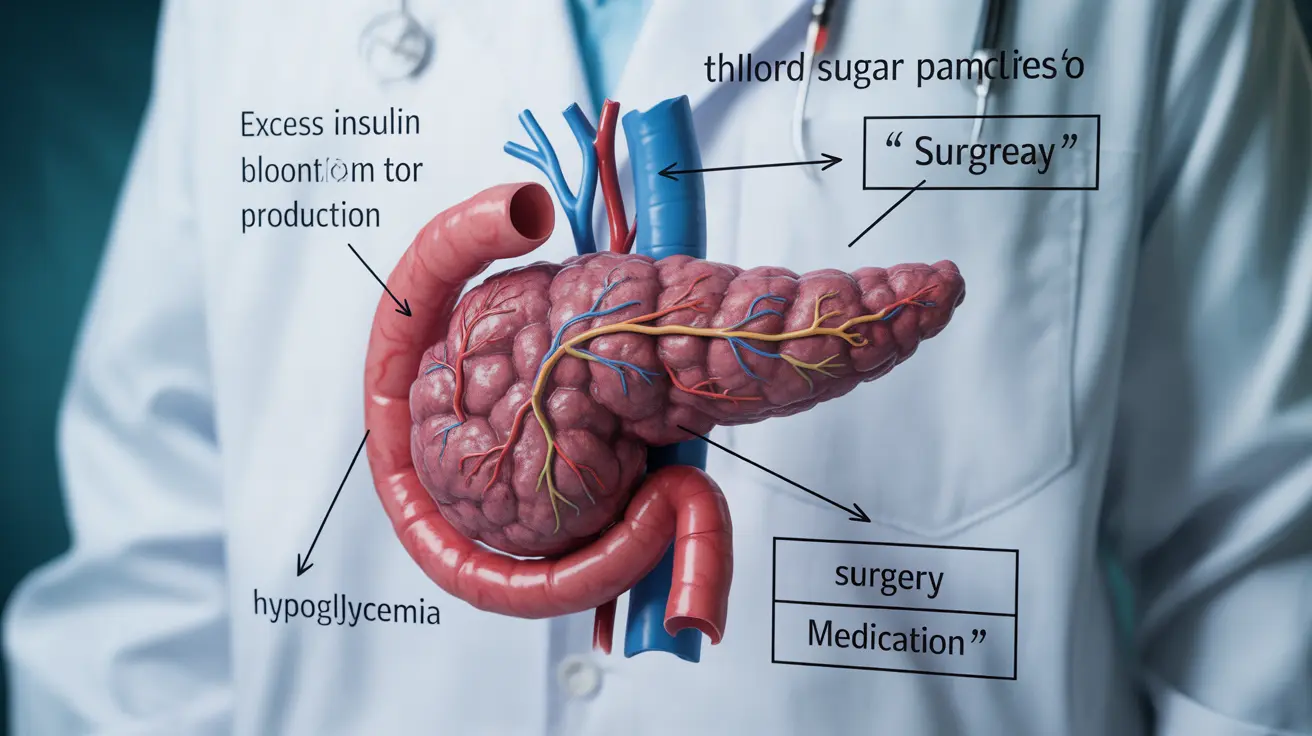
Insulinoma is a rare but significant type of pancreatic tumor that produces excess insulin, leading to potentially serious complications in blood sugar regulation. These tumors, while usually benign, can significantly impact a person's quality of life and require careful medical attention for proper diagnosis and management.
Understanding insulinoma is crucial for both healthcare providers and patients, as early recognition of symptoms can lead to better outcomes. This comprehensive guide explores the key aspects of insulinoma, from its characteristic symptoms to available treatment options.
Key Symptoms of Insulinoma
The symptoms of insulinoma primarily result from excess insulin production, which leads to low blood sugar (hypoglycemia). Common signs include:
- Confusion and difficulty concentrating
- Unusual sweating, especially during fasting
- Trembling or shakiness
- Weakness and fatigue
- Episodes of hunger
- Anxiety or panic attacks
- Visual disturbances
- Heart palpitations
These symptoms typically become more pronounced when fasting or between meals, and may improve after eating. Some patients might experience more severe symptoms, including loss of consciousness or seizures if blood sugar drops too low.
Diagnostic Process and Testing
Diagnosing insulinoma requires a systematic approach combining various medical tests and procedures:
Blood Tests and Monitoring
Healthcare providers typically start with:
- Fasting blood glucose tests
- 72-hour fasting test
- Insulin level measurements
- C-peptide level testing
Imaging Studies
Several imaging techniques help locate and characterize the tumor:
- CT scans with contrast
- MRI imaging
- Endoscopic ultrasound
- Nuclear medicine scans
- Specialized PET scans
Treatment Approaches
Treatment for insulinoma primarily focuses on removing the tumor and managing blood sugar levels. The main options include:
Surgical Management
Surgery remains the primary and most effective treatment for most insulinoma cases. Surgical approaches may include:
- Laparoscopic tumor removal
- Traditional open surgery
- Partial pancreatic resection when necessary
Medical Management
When surgery isn't immediately possible or during preparation for surgery, medical treatments may include:
- Diazoxide to control blood sugar
- Regular meals and snacks
- Glucose monitoring
- Emergency glucose treatments
Managing Blood Sugar Episodes
Patients with insulinoma need to be prepared for hypoglycemic episodes. Important management strategies include:
- Carrying fast-acting glucose sources
- Regular blood sugar monitoring
- Meal planning and timing
- Having glucagon injection kits available
- Wearing medical alert jewelry
Frequently Asked Questions
What are the common symptoms that suggest I might have an insulinoma? Common symptoms include frequent episodes of low blood sugar, confusion, unusual sweating, trembling, weakness, and hunger. These symptoms often occur during fasting or between meals and improve after eating.
How is insulinoma diagnosed and what tests are involved? Diagnosis typically involves blood tests, including a 72-hour fasting test, insulin and C-peptide measurements, and various imaging studies such as CT scans, MRI, and endoscopic ultrasound to locate the tumor.
What treatment options are available for insulinoma and how effective is surgery? Surgery is the most effective treatment option, with success rates over 90% when the tumor can be completely removed. Surgical options include laparoscopic or traditional open surgery. Medical management with medications may be used when surgery isn't immediately possible.
Can insulinomas cause severe low blood sugar episodes, and how can these be managed? Yes, insulinomas can cause severe hypoglycemic episodes. Management includes regular monitoring of blood sugar, carrying fast-acting glucose sources, maintaining regular meal schedules, and having emergency glucose or glucagon available.
Are there genetic or risk factors that increase the chance of developing insulinoma? While most insulinomas occur sporadically, some cases are associated with Multiple Endocrine Neoplasia type 1 (MEN1) syndrome, a genetic condition. Age and family history may play a role in development risk.