Laryngospasm is a sudden, involuntary spasm of the vocal cords that temporarily blocks the airway, making it difficult or impossible to breathe or speak. This frightening experience can occur without warning and may last anywhere from a few seconds to several minutes. While laryngospasm episodes are typically brief and resolve on their own, understanding this condition is crucial for anyone who experiences these episodes or cares for someone who does.
Though laryngospasm can be alarming, most cases are not life-threatening and can be managed effectively with proper knowledge and techniques. Learning about the triggers, symptoms, and treatment approaches can help individuals feel more prepared and confident when dealing with this condition.
What Causes Laryngospasm?
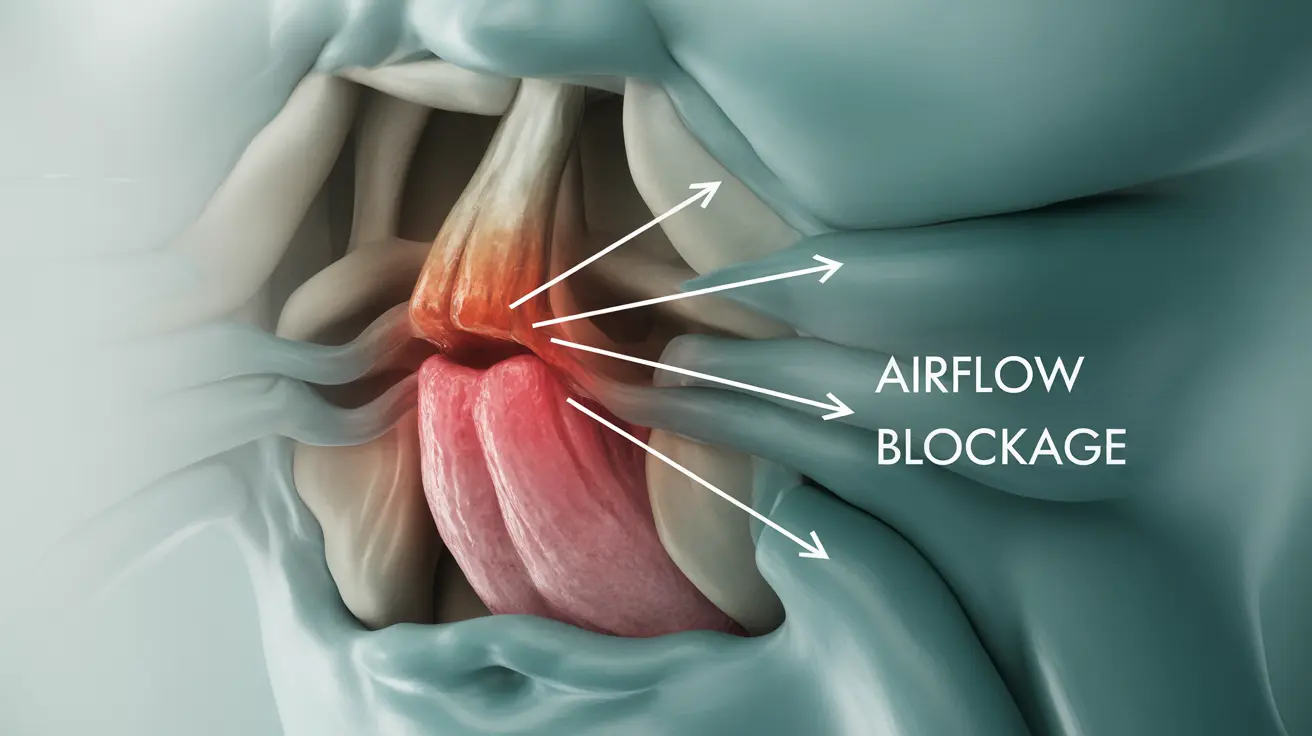
Laryngospasm occurs when the muscles controlling the vocal cords contract suddenly and involuntarily, causing the vocal cords to close tightly. This spasm can be triggered by various factors, ranging from medical procedures to underlying health conditions.
Common medical triggers include anesthesia during surgery, particularly when breathing tubes are inserted or removed. The larynx is highly sensitive to irritation, and medical instruments can easily provoke a spasm response. Intubation and extubation procedures carry the highest risk, especially in patients with pre-existing respiratory conditions.
Environmental and lifestyle factors also play significant roles in triggering laryngospasm episodes. Strong chemical odors, cigarette smoke, dust, and other airborne irritants can cause the vocal cords to spasm defensively. Cold air, particularly during winter months or in air-conditioned environments, may also trigger episodes in sensitive individuals.
Certain medical conditions increase the likelihood of experiencing laryngospasm. Gastroesophageal reflux disease (GERD) is one of the most common underlying causes, as stomach acid can irritate the larynx when it travels upward. Asthma, allergies, and upper respiratory infections can also make the vocal cords more reactive and prone to spasms.
Recognizing Laryngospasm Symptoms
The primary symptom of laryngospasm is sudden difficulty breathing, often described as feeling like the throat has completely closed off. This sensation can be extremely frightening, particularly for first-time sufferers who may feel like they're choking or suffocating.
During an episode, individuals typically cannot speak or make vocal sounds because the vocal cords are tightly closed. Breathing becomes labored or impossible through the mouth, though some air may still pass through the nose. The person may instinctively grab their throat or assume a forward-leaning position to try to open the airway.
Physical symptoms often accompany the breathing difficulties. Many people experience a high-pitched sound when trying to inhale, similar to stridor. The chest may feel tight, and there might be a sensation of panic or anxiety as the body responds to the perceived threat of not being able to breathe.
In some cases, laryngospasm may be accompanied by coughing fits before or after the main episode. The skin around the lips and fingernails might appear slightly blue (cyanosis) due to temporary oxygen restriction, though this typically resolves quickly once normal breathing resumes.
Effective Treatment and Management Strategies
The immediate treatment for laryngospasm focuses on helping the vocal cords relax and restoring normal breathing. The most effective initial approach is to remain calm and try specific breathing techniques that can help break the spasm cycle.
One proven technique involves breathing in slowly through the nose while keeping the mouth closed. This method helps bypass the closed vocal cords and can sometimes help them relax. Another approach is to hold the breath for a few seconds, then slowly exhale through pursed lips, which may help reset the laryngeal muscles.
For severe or prolonged episodes, medical intervention may be necessary. Healthcare providers might administer continuous positive airway pressure (CPAP) or use medications such as muscle relaxants to help stop the spasm. In emergency situations, procedures to establish an alternative airway might be required, though this is extremely rare.
Long-term management often involves identifying and avoiding personal triggers. Keeping a symptom diary can help pinpoint specific environmental factors or situations that tend to provoke episodes. This information becomes invaluable for developing personalized prevention strategies.
For individuals with frequent episodes, working with healthcare providers to address underlying conditions is essential. Treatment might include acid reflux management, allergy control, or respiratory therapy techniques to strengthen and coordinate the muscles involved in breathing and swallowing.
Prevention and Lifestyle Modifications
Preventing laryngospasm often involves making targeted lifestyle changes based on individual triggers. For those with GERD-related episodes, dietary modifications such as avoiding spicy foods, caffeine, and large meals before bedtime can significantly reduce frequency.
Environmental control measures include using air purifiers to reduce irritants, avoiding strong fragrances or cleaning products, and staying hydrated to keep the throat tissues moist. During cold weather, covering the nose and mouth with a scarf can help warm and humidify incoming air.
Stress management techniques such as meditation, yoga, or regular exercise may help reduce overall muscle tension and make laryngospasm episodes less likely. Some individuals benefit from working with speech-language pathologists to learn specific vocal exercises and breathing techniques.
Frequently Asked Questions
What are the common causes and triggers of laryngospasm?
Laryngospasm can be triggered by medical procedures involving the airway, environmental irritants like smoke or strong odors, cold air, and underlying conditions such as GERD, asthma, or respiratory infections. Anesthesia and intubation during surgery are among the most common medical triggers, while everyday triggers include chemical fumes, dust, and sudden temperature changes.
What symptoms should I look for during a laryngospasm episode?
The main symptoms include sudden difficulty breathing, inability to speak or make sounds, a feeling that the throat has closed completely, and possible high-pitched sounds when trying to inhale. You might also experience chest tightness, panic, and in some cases, slight bluish coloring around the lips due to temporary oxygen restriction. Episodes typically last seconds to minutes.
How can laryngospasm be treated and managed effectively?
Immediate treatment involves staying calm and breathing slowly through the nose with the mouth closed. Holding your breath briefly, then exhaling slowly through pursed lips can also help. For severe episodes, medical treatment may include CPAP therapy or muscle relaxants. Long-term management focuses on identifying triggers, treating underlying conditions, and learning specific breathing techniques.
Can gastroesophageal reflux disease (GERD) cause laryngospasm?
Yes, GERD is one of the most common underlying causes of laryngospasm. When stomach acid travels upward and reaches the larynx, it can irritate the vocal cords and trigger spasms. Managing GERD through dietary changes, medications, and lifestyle modifications can significantly reduce laryngospasm episodes in affected individuals.
When should I see a doctor if I experience laryngospasm?
Seek immediate medical attention if episodes are severe, last longer than a few minutes, or occur frequently. You should also consult a healthcare provider if laryngospasm interferes with daily activities, is accompanied by other concerning symptoms, or if you suspect an underlying condition like GERD or asthma might be contributing to the episodes.