Leukocytosis is a medical condition characterized by an elevated white blood cell count in the blood. This increase in white blood cells (leukocytes) often indicates that your body is fighting an infection, inflammation, or other underlying health conditions. Understanding the causes, symptoms, and treatment options for leukocytosis is crucial for proper medical management.
While a temporary elevation in white blood cells can be a normal response to infection or stress, persistent leukocytosis requires medical attention to determine and address its root cause. This comprehensive guide will explore the various aspects of this condition and what you need to know.
Types and Causes of Leukocytosis
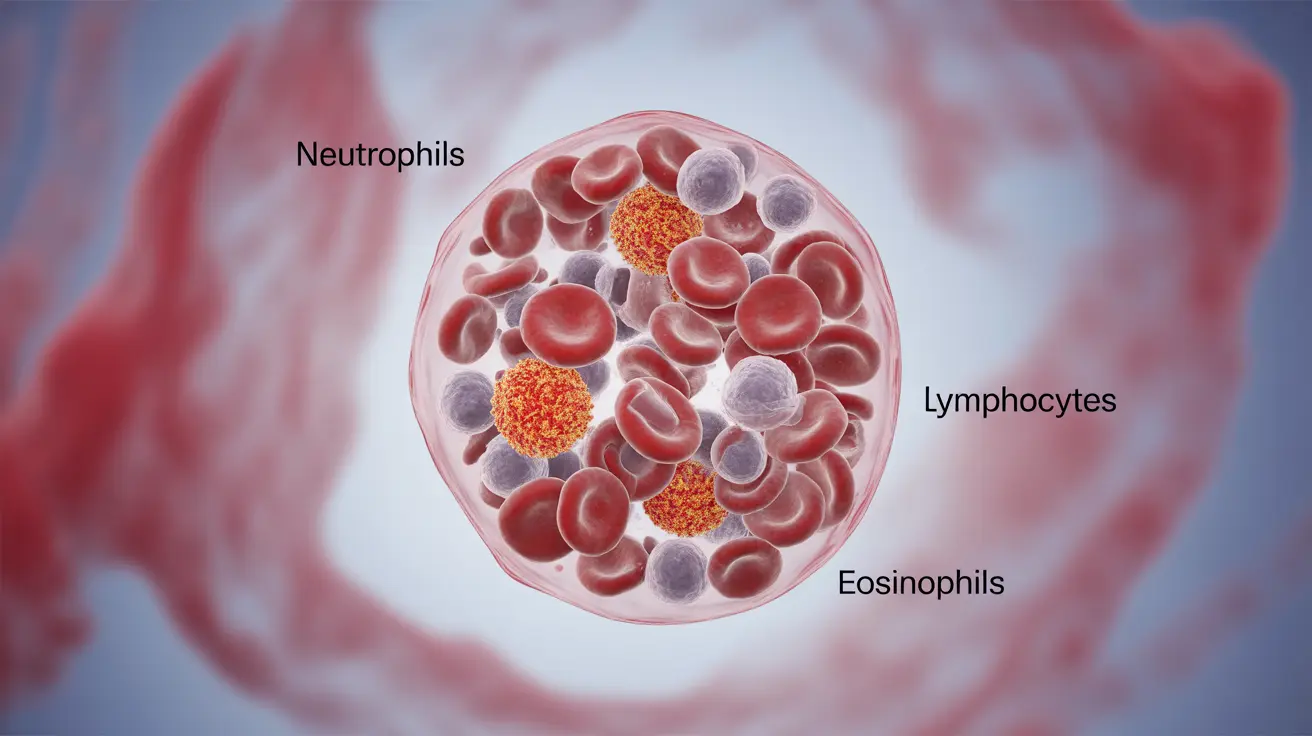
Leukocytosis can involve different types of white blood cells, each indicating specific underlying conditions:
Neutrophilic Leukocytosis
The most common form, characterized by increased neutrophils, typically indicates:
- Bacterial infections
- Tissue injury or trauma
- Inflammatory conditions
- Certain medications
- Stress response
Lymphocytic Leukocytosis
An increase in lymphocytes may suggest:
- Viral infections
- Chronic infections
- Certain types of leukemia
- Autoimmune disorders
Eosinophilic Leukocytosis
Elevated eosinophils often point to:
- Allergic reactions
- Parasitic infections
- Asthma
- Certain skin conditions
Common Symptoms Associated with Leukocytosis
The symptoms of leukocytosis often reflect its underlying cause rather than the condition itself. Common signs may include:
- Fever
- Fatigue
- Body aches
- Swollen lymph nodes
- Night sweats
- Unexplained weight loss
- Frequent infections
Diagnostic Process
Diagnosing leukocytosis involves several steps:
Initial Blood Tests
A complete blood count (CBC) is the primary diagnostic tool, measuring:
- Total white blood cell count
- Differential count of specific white blood cell types
- Other blood cell parameters
Additional Testing
Based on initial findings, doctors may recommend:
- Blood smear examination
- Bone marrow biopsy
- Imaging studies
- Specific tests for suspected underlying conditions
Treatment Approaches
Treatment for leukocytosis focuses on addressing its underlying cause:
Infection-Related Treatment
- Antibiotics for bacterial infections
- Antiviral medications when appropriate
- Supportive care measures
Inflammatory Condition Management
- Anti-inflammatory medications
- Immunosuppressants when necessary
- Lifestyle modifications
Chronic Condition Care
For ongoing management of underlying conditions, treatment may include:
- Regular monitoring
- Medication adjustments
- Lifestyle changes
- Prevention strategies
Frequently Asked Questions
What are the most common causes of leukocytosis and how do they differ by white blood cell type?
The most common causes vary by white blood cell type. Neutrophilic leukocytosis typically results from bacterial infections or inflammation. Lymphocytic leukocytosis often indicates viral infections or lymphoid malignancies. Eosinophilic leukocytosis usually suggests allergic reactions or parasitic infections.
What symptoms should I watch for if I have a high white blood cell count?
Key symptoms to monitor include persistent fever, unexplained fatigue, frequent infections, night sweats, and unexplained weight loss. Any new or worsening symptoms should be reported to your healthcare provider.
How is leukocytosis diagnosed through blood tests and what additional exams might be needed?
Diagnosis begins with a complete blood count (CBC) and differential count. Additional tests may include blood smears, bone marrow biopsies, imaging studies, and specific tests based on suspected underlying conditions.
What treatments are available for leukocytosis based on its underlying cause?
Treatment options depend on the underlying cause and may include antibiotics for bacterial infections, anti-inflammatory medications for inflammatory conditions, or specific treatments for chronic conditions. Some cases may require ongoing monitoring and management.
How can I prevent leukocytosis or manage chronic high white blood cell levels safely?
Prevention and management strategies include maintaining good hygiene, following prescribed treatment plans, regular medical check-ups, stress management, and adopting a healthy lifestyle. People with chronic conditions should work closely with their healthcare providers to develop appropriate management plans.