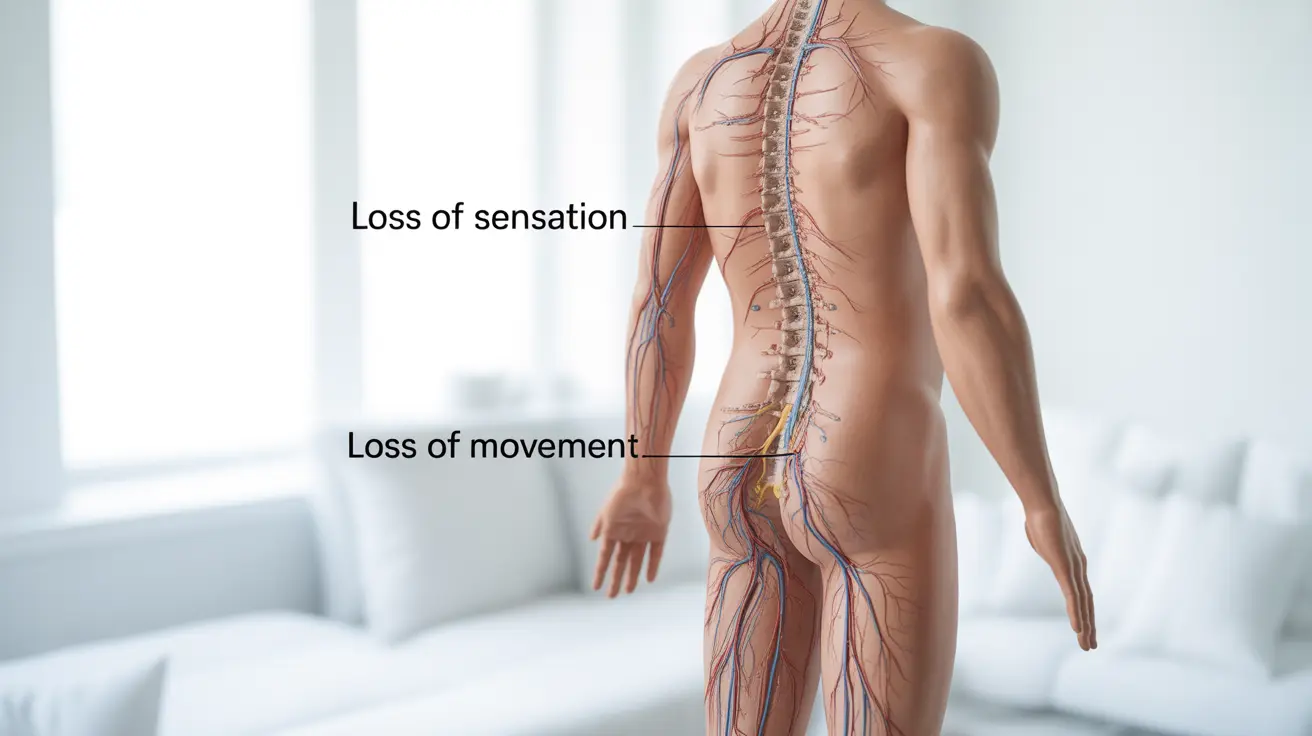
Paraplegia is a serious medical condition characterized by the loss of sensation and movement in the lower body, significantly impacting a person's daily life and mobility. This condition typically affects both legs, pelvic organs, and lower parts of the torso, depending on the location of the injury or condition causing the paralysis.
Understanding paraplegia is crucial for both those affected and their caregivers, as it involves complex care requirements and lifestyle adaptations. This comprehensive guide explores the causes, symptoms, diagnosis, and management strategies for paraplegia.
Common Causes and Prevention of Paraplegia
Paraplegia can result from various circumstances, with trauma being the leading cause. The most common causes include:
- Spinal cord injuries from accidents
- Tumors affecting the spinal cord
- Infectious diseases
- Congenital conditions
- Vascular problems affecting spinal blood flow
Prevention strategies focus primarily on safety measures and lifestyle choices:
- Using appropriate safety equipment during sports and activities
- Practicing proper workplace safety
- Following traffic safety rules
- Maintaining good spinal health
- Regular medical check-ups for early detection of potential issues
Symptoms and Clinical Manifestations
The symptoms of paraplegia can vary depending on the level of injury and extent of damage to the spinal cord. Common symptoms include:
- Loss of movement in the legs
- Absence of sensation below the injury level
- Loss of bladder and bowel control
- Sexual dysfunction
- Muscle spasms
- Changes in reflexes
- Potential respiratory difficulties
Secondary Complications
People with paraplegia may experience several secondary conditions that require careful monitoring:
- Pressure sores
- Deep vein thrombosis
- Respiratory infections
- Urinary tract infections
- Chronic pain
- Depression and anxiety
Diagnostic Approach
Diagnosing paraplegia involves a comprehensive medical evaluation using various diagnostic tools and procedures:
- Detailed neurological examination
- Magnetic Resonance Imaging (MRI)
- Computed Tomography (CT) scans
- X-rays
- Electromyography (EMG)
- Blood tests to rule out other conditions
Treatment and Rehabilitation Strategies
Treatment for paraplegia typically involves a multi-disciplinary approach:
Medical Management
- Medication for pain and spasticity
- Surgery when necessary
- Prevention and treatment of complications
- Regular medical monitoring
Physical Rehabilitation
Physical therapy plays a crucial role in maintaining function and preventing complications:
- Range of motion exercises
- Strength training
- Transfer training
- Balance exercises
- Gait training when appropriate
Assistive Devices and Technology
Various assistive devices can help improve independence:
- Manual and powered wheelchairs
- Transfer equipment
- Modified vehicles
- Adaptive home equipment
- Computer access technology
Lifestyle Modifications and Independence
Successful adaptation to life with paraplegia often requires significant lifestyle changes:
- Home modifications for accessibility
- Development of new daily living strategies
- Regular exercise routines
- Proper nutrition and weight management
- Strong support system development
Frequently Asked Questions
What are the most common causes of paraplegia and how can they be prevented?
The most common causes include traumatic injuries, particularly from vehicle accidents, falls, and sports injuries. Prevention involves using proper safety equipment, following traffic rules, and maintaining workplace safety protocols. Regular exercise and maintaining good spinal health can also help prevent some non-traumatic causes.
What symptoms can I expect if I have paraplegia, and how are they managed?
Primary symptoms include loss of movement and sensation in the lower body, bladder and bowel changes, and potential sexual dysfunction. Management involves a combination of medications, physical therapy, and assistive devices, along with regular monitoring for complications.
How is paraplegia diagnosed, and what are the typical tests used?
Diagnosis typically involves a thorough neurological examination, imaging tests like MRI and CT scans, and other specialized tests such as EMG. These help determine the location and extent of the spinal cord injury or condition causing paraplegia.
What are the most effective treatments and assistive devices for managing paraplegia?
Effective treatments include comprehensive rehabilitation programs, medications for symptom management, and various assistive devices such as wheelchairs and transfer equipment. The specific combination depends on the individual's needs and level of injury.
How can lifestyle changes and physical therapy help improve mobility and independence in people with paraplegia?
Regular physical therapy helps maintain muscle strength and prevent complications, while lifestyle modifications like home adaptations and learning new techniques for daily activities can significantly improve independence. A balanced diet, regular exercise, and strong social support are also crucial for optimal outcomes.