Placental insufficiency is a serious pregnancy complication where the placenta doesn't function properly, potentially affecting your baby's growth and development. This condition occurs when the placenta, the vital organ that supplies nutrients and oxygen to your growing baby, fails to deliver adequate support throughout pregnancy.
Understanding placental insufficiency is crucial for expectant mothers and healthcare providers alike, as early detection and proper management can significantly improve outcomes for both mother and baby.
What is Placental Insufficiency?
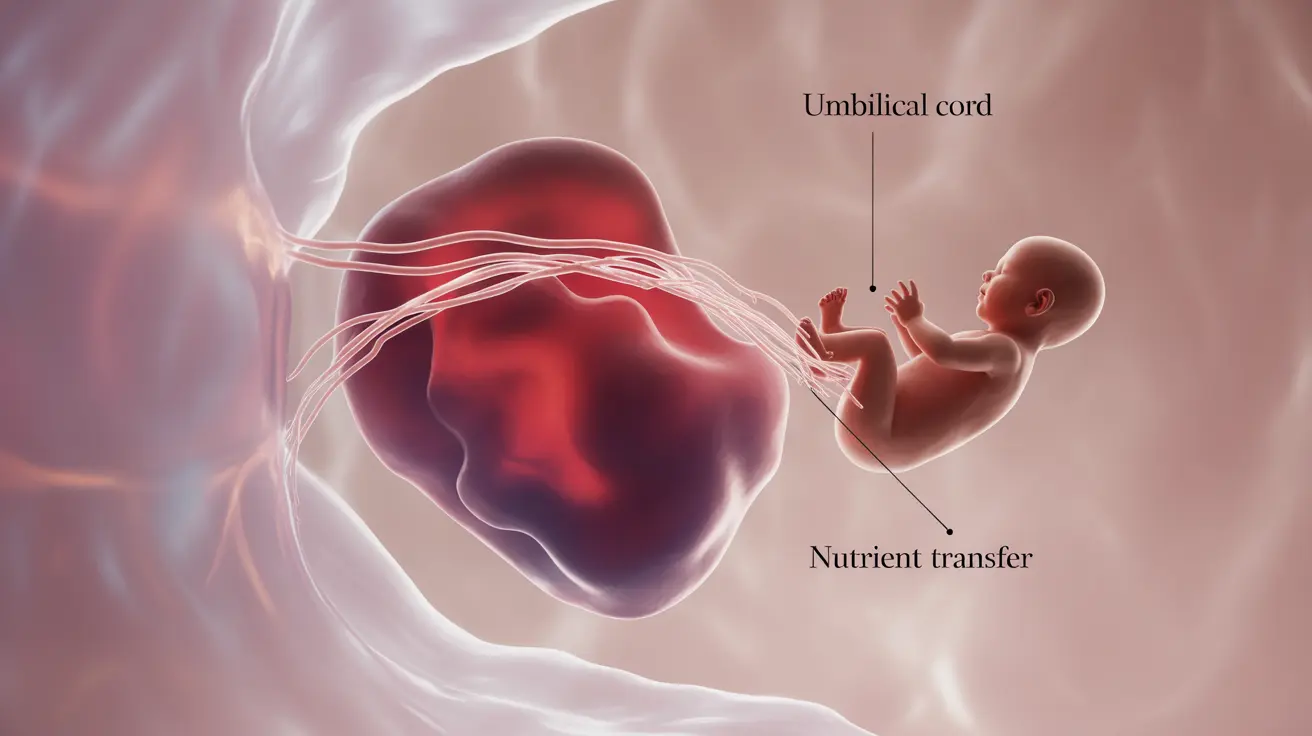
Placental insufficiency, also known as placental dysfunction or uteroplacental insufficiency, occurs when the placenta cannot provide sufficient nutrients and oxygen to support optimal fetal growth. This vital organ, which develops during pregnancy, acts as your baby's lifeline, facilitating essential exchanges between maternal and fetal circulation.
Risk Factors and Causes
Several factors can contribute to the development of placental insufficiency:
- Maternal health conditions (chronic hypertension, diabetes, or blood clotting disorders)
- Advanced maternal age
- Multiple pregnancies
- Previous uterine conditions or surgeries
- Substance use (smoking, alcohol, or drugs)
- Certain autoimmune disorders
Common Signs and Symptoms
Identifying placental insufficiency early is critical for proper management. Key indicators include:
- Decreased fetal movement
- Smaller than expected fundal height
- Poor fetal growth detected during ultrasounds
- Abnormal pregnancy test results
- Lower than normal amniotic fluid levels
Diagnostic Approaches
Healthcare providers use various methods to diagnose and monitor placental insufficiency:
Ultrasound Monitoring
Regular ultrasound scans help track fetal growth and assess placental health. Doppler ultrasound specifically evaluates blood flow through the placenta and umbilical cord.
Physical Examinations
Healthcare providers regularly measure fundal height and monitor fetal movement patterns to detect potential issues early.
Management and Treatment Strategies
While placental insufficiency cannot be directly treated, several management approaches can help protect your baby's health:
- Close monitoring through frequent prenatal visits
- Bed rest or reduced activity when recommended
- Careful management of underlying health conditions
- Possible hospitalization for severe cases
- Timing delivery based on fetal well-being and gestational age
Frequently Asked Questions
- What causes placental insufficiency during pregnancy?
Placental insufficiency can be caused by various factors including maternal health conditions (such as hypertension or diabetes), blood clotting disorders, advanced maternal age, smoking, and multiple pregnancies. Sometimes, the exact cause remains unknown.
- What signs or symptoms might indicate placental insufficiency in my pregnancy?
Key signs include decreased fetal movement, smaller than expected fundal height measurements, poor fetal growth on ultrasounds, and reduced amniotic fluid levels. Regular prenatal check-ups help monitor these indicators.
- How is placental insufficiency diagnosed and monitored by healthcare providers?
Healthcare providers use a combination of ultrasound scans (including Doppler ultrasound), physical examinations, fundal height measurements, and fetal movement monitoring. Regular prenatal testing helps track the condition's progression.
- What are the potential risks and complications of placental insufficiency for my baby and me?
Risks include intrauterine growth restriction, preterm birth, low birth weight, and in severe cases, pregnancy loss. For mothers, there may be an increased risk of cesarean delivery and pregnancy complications.
- How can placental insufficiency be managed or treated to protect my baby's health?
Management typically involves close monitoring, possible activity modification, treating underlying conditions, and timing delivery appropriately. Some cases may require hospitalization for intensive monitoring and care.