Rectal pain can be an uncomfortable and concerning symptom that affects many people at some point in their lives. While this condition may cause anxiety, understanding its common causes, symptoms, and treatment options can help you better manage your health and know when to seek medical attention.
This comprehensive guide will explore the various causes of rectal pain, how to identify them, and effective treatment approaches. We'll also discuss important lifestyle modifications that can help prevent and alleviate discomfort.
Common Causes of Rectal Pain
Rectal pain can stem from several different conditions, each with distinct characteristics and treatment needs:
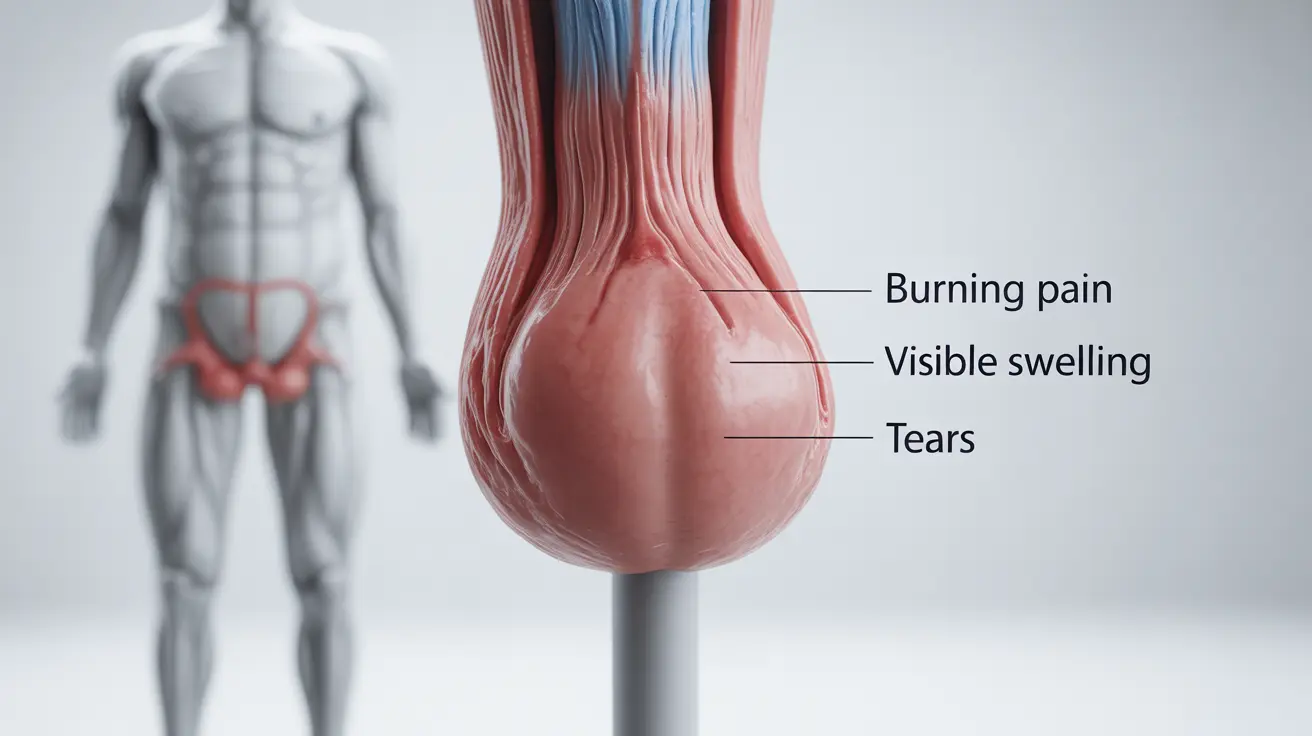
Hemorrhoids
Hemorrhoids are swollen blood vessels in the rectal area that can cause:
- Burning or throbbing pain
- Discomfort during bowel movements
- Itching and irritation
- Visible swelling around the anus
Anal Fissures
These small tears in the anal canal lining typically cause:
- Sharp, burning pain during bowel movements
- Pain that can last several hours after defecation
- Small amounts of bright red bleeding
- Visible crack or tear in the anal area
Other Common Causes
Additional conditions that may lead to rectal pain include:
- Proctitis (inflammation of the rectum)
- Levator ani syndrome
- Proctalgia fugax
- Anal abscesses
- Sexually transmitted infections
Diagnostic Approaches
Healthcare providers use various methods to diagnose the cause of rectal pain:
Physical Examination
A thorough physical exam often includes:
- Visual inspection of the anal area
- Digital rectal examination
- Anoscopy when necessary
Additional Testing
Depending on symptoms, doctors may recommend:
- Colonoscopy
- Sigmoidoscopy
- Imaging studies
- Blood tests
Treatment Options
Treatment approaches vary based on the underlying cause but may include:
Conservative Treatments
- Sitz baths
- Over-the-counter pain relievers
- Topical treatments
- Lifestyle modifications
- Dietary changes
Medical Interventions
More severe cases might require:
- Prescription medications
- Minimally invasive procedures
- Surgical treatment in some cases
Prevention Strategies
Several lifestyle modifications can help prevent rectal pain:
Dietary Considerations
- Increase fiber intake
- Stay well-hydrated
- Avoid irritating foods
- Maintain regular eating habits
Lifestyle Habits
- Practice good bathroom habits
- Avoid straining during bowel movements
- Exercise regularly
- Maintain good hygiene
Frequently Asked Questions
What are the most common causes of rectal pain and how can I tell them apart? The most common causes are hemorrhoids and anal fissures. Hemorrhoids typically cause throbbing pain and itching, while fissures cause sharp pain during bowel movements that may last for hours afterward.
How is rectal pain from hemorrhoids different from pain caused by anal fissures? Hemorrhoid pain tends to be dull and throbbing with itching, while anal fissure pain is usually sharp and intense, particularly during and after bowel movements.
What treatments are available for relieving rectal pain caused by hemorrhoids or anal fissures? Treatment options include sitz baths, over-the-counter pain relievers, topical treatments, and lifestyle modifications. Severe cases may require medical procedures or surgery.
When should I see a doctor for rectal pain and what tests might they perform? Seek medical attention if pain is severe, persistent, or accompanied by bleeding. Doctors typically perform physical examinations and may recommend additional tests like anoscopy or colonoscopy.
How can diet and lifestyle changes help prevent or reduce rectal pain? Maintaining a high-fiber diet, staying hydrated, practicing good bathroom habits, and regular exercise can help prevent and reduce rectal pain. Avoiding straining during bowel movements is also crucial.
Remember, while rectal pain is common, persistent or severe symptoms should always be evaluated by a healthcare professional to ensure proper diagnosis and treatment.