Regurgitation, the backflow of stomach contents into the mouth or throat, can be an uncomfortable and distressing symptom that affects many people. While commonly associated with gastroesophageal reflux disease (GERD), regurgitation can stem from various causes and significantly impact daily life and sleep quality. Understanding its underlying causes and available treatment options is crucial for effective management.
This comprehensive guide explores the various aspects of regurgitation, from its common symptoms and causes to practical prevention strategies and treatment approaches. Whether you're experiencing occasional episodes or frequent occurrences, this information will help you better understand and manage this condition.
Understanding Regurgitation and Its Symptoms
Regurgitation manifests differently from typical acid reflux or heartburn. The primary characteristics include:
- A sour or bitter taste in the mouth
- The sensation of food or liquid moving up the throat
- Undigested food particles returning to the mouth
- Little to no burning sensation (unlike heartburn)
- A wet burp or mild vomiting feeling
These symptoms often occur shortly after eating and can be particularly troublesome when lying down or bending over. Unlike vomiting, regurgitation typically happens without nausea or forceful muscle contractions.
Common Causes Beyond GERD
While GERD is a primary cause of regurgitation, several other conditions can trigger this symptom:
- Hiatal hernia
- Gastroparesis (delayed stomach emptying)
- Pregnancy
- Eating disorders
- Rumination syndrome
- Esophageal motility disorders
Prevention Through Lifestyle Changes
Several lifestyle modifications can help prevent or reduce regurgitation episodes:
Dietary Adjustments
Making smart food choices can significantly impact symptom frequency:
- Avoid trigger foods (spicy, fatty, or acidic items)
- Eat smaller, more frequent meals
- Stop eating 2-3 hours before bedtime
- Maintain a healthy weight
Posture and Timing
Simple behavioral changes can make a difference:
- Stay upright after meals for at least 30 minutes
- Elevate the head of your bed by 6-8 inches
- Avoid tight-fitting clothes
- Practice proper eating habits and thorough chewing
Treatment Approaches
Treatment options vary depending on the underlying cause and severity of symptoms:
Medical Interventions
- Proton pump inhibitors (PPIs)
- H2 blockers
- Prokinetic medications
- Antacids for immediate relief
Professional Support
In some cases, working with healthcare providers may be necessary:
- Gastroenterologist consultation
- Physical therapy for specific conditions
- Behavioral therapy for rumination syndrome
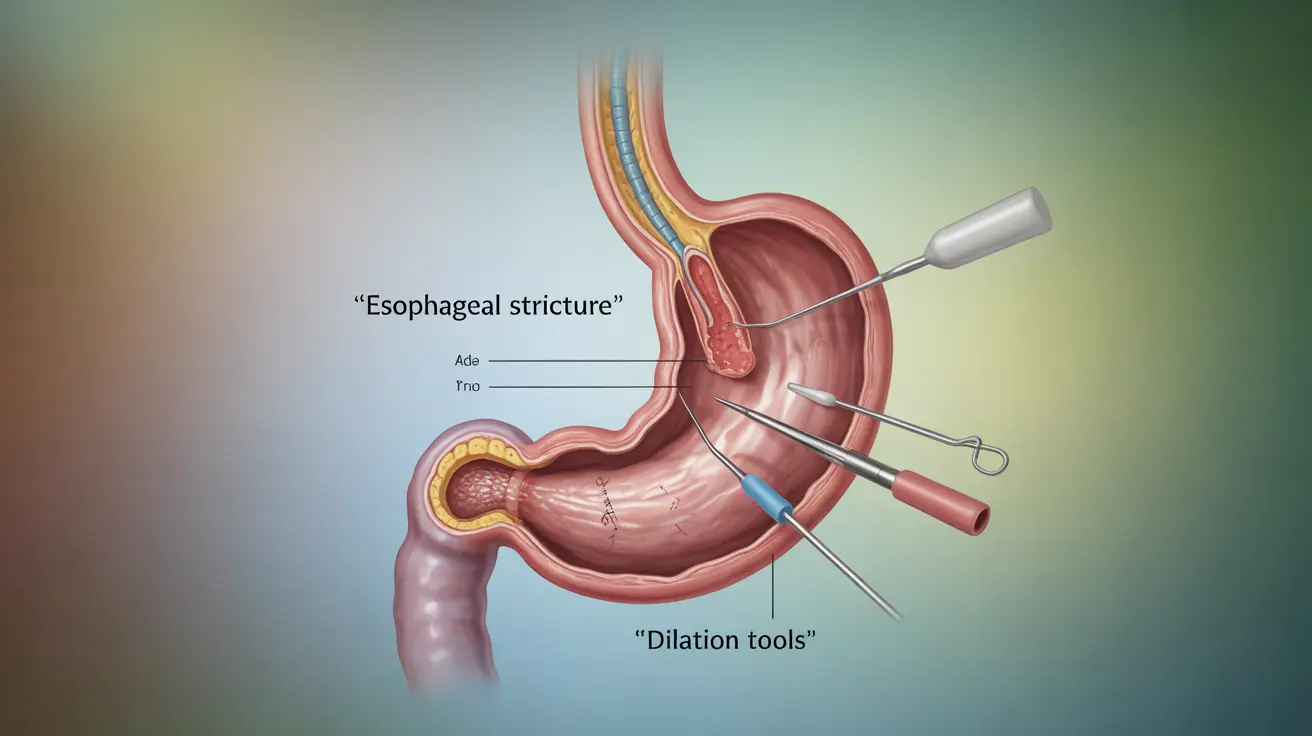
- Surgical options for severe cases
Managing Nighttime Regurgitation
Nighttime regurgitation can significantly affect sleep quality. Implement these strategies for better rest:
- Use a wedge pillow or bed risers
- Avoid late-night snacking
- Sleep on your left side
- Consider gravity-based positioning techniques
Frequently Asked Questions
What are the typical symptoms of regurgitation, and how does it relate to GERD? Regurgitation symptoms include the backflow of food or liquid into the mouth or throat, often accompanied by a sour taste. It's a common symptom of GERD, occurring when the lower esophageal sphincter doesn't function properly.
How can I prevent regurgitation naturally through diet and lifestyle changes? Natural prevention methods include eating smaller meals, avoiding trigger foods, maintaining an upright position after eating, and not lying down for 2-3 hours after meals. Weight management and stress reduction can also help.
What are the most effective treatments for frequent regurgitation in adults? Effective treatments include medications like PPIs or H2 blockers, lifestyle modifications, and in some cases, surgical interventions. The best treatment depends on the underlying cause and severity of symptoms.
Can regurgitation be caused by anything other than GERD, and what are those conditions? Yes, regurgitation can be caused by conditions such as hiatal hernia, gastroparesis, pregnancy, eating disorders, rumination syndrome, and various esophageal motility disorders.
How can I manage regurgitation at night to improve sleep quality? Nighttime regurgitation can be managed by elevating the head of the bed, using wedge pillows, avoiding late meals, sleeping on the left side, and maintaining good sleep hygiene practices.