When arteries become narrowed or blocked due to various cardiovascular conditions, medical professionals often turn to stents as a crucial solution. These small, mesh-like tubes play a vital role in keeping blood vessels open and maintaining healthy blood flow throughout the body. Understanding how stents work and what to expect during the procedure can help patients feel more confident about their treatment journey.
This comprehensive guide explores everything you need to know about stents, from their basic function to recovery expectations and long-term care considerations. Whether you're preparing for a stent procedure or simply seeking information, we'll cover the essential aspects of this life-saving medical intervention.
What Is a Stent and How Does It Work?
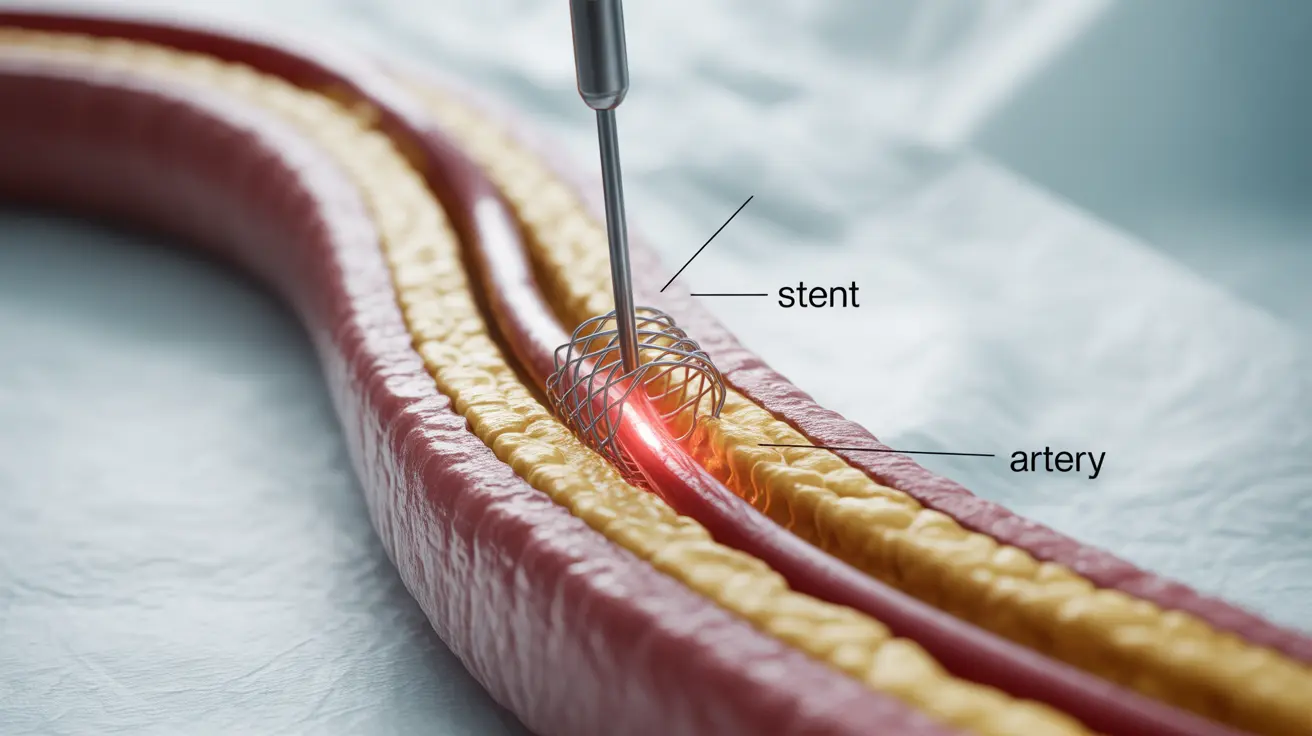
A stent is a tiny, expandable tube made of metal mesh that serves as a scaffold to keep arteries open. During placement, the stent is initially compressed and mounted on a balloon catheter. When the catheter reaches the blocked or narrowed area, the balloon inflates, expanding the stent against the artery walls. The stent remains in place permanently, holding the artery open and allowing blood to flow freely.
Types of Stents
Bare Metal Stents
These traditional stents are simple metal mesh tubes that provide basic structural support to keep arteries open. They're typically less expensive than other options but may have a higher risk of restenosis (re-narrowing of the artery).
Drug-Eluting Stents
These advanced stents are coated with medication that slowly releases into the artery wall. The medication helps prevent scar tissue formation, significantly reducing the risk of restenosis. While more expensive, they often provide better long-term outcomes for many patients.
The Stent Placement Procedure
Stent placement typically occurs during an angioplasty procedure, which is performed under local anesthesia. The doctor makes a small incision, usually in the groin or arm, to access the affected artery. Using X-ray guidance, they thread a catheter through the blood vessels to the blocked area. The stent is then deployed, and the catheter is removed.
Recovery and Aftercare
Recovery from stent placement varies by patient and procedure type, but most people can return home within 24 hours. The initial recovery period typically lasts several days to a week, during which patients should:
- Rest and gradually increase activity levels
- Keep the insertion site clean and dry
- Take prescribed medications as directed
- Monitor for any unusual symptoms
- Follow dietary and lifestyle recommendations
Preventing Complications and Maintaining Stent Health
Long-term success with stents requires ongoing care and lifestyle modifications. Key preventive measures include:
- Taking prescribed blood-thinning medications
- Maintaining a heart-healthy diet
- Regular exercise as approved by your doctor
- Quitting smoking
- Managing underlying conditions like diabetes or high blood pressure
- Regular follow-up appointments with healthcare providers
Frequently Asked Questions
What is a stent and how does it help open blocked arteries during angioplasty?
A stent is a small, mesh-like tube that acts as a permanent scaffold to keep arteries open. During angioplasty, the stent is delivered via catheter and expanded at the blockage site, pressing against the artery walls to maintain proper blood flow.
How long does it take to recover after a peripheral artery stent placement?
Most patients can return home within 24 hours after the procedure. Initial recovery typically takes 5-7 days, though full recovery may take several weeks. Patients can usually resume normal activities within a week, following their doctor's guidance.
What are the risks and potential complications of stent placement in leg arteries?
Potential complications include bleeding, infection, blood clots, allergic reactions to medications or dye, artery damage, and restenosis. While these risks exist, serious complications are relatively rare when procedures are performed by experienced healthcare providers.
What are the differences between drug-eluting stents and bare metal stents?
Drug-eluting stents have a medication coating that helps prevent scar tissue formation and reduces the risk of restenosis. Bare metal stents provide basic structural support but don't have this medication coating. Drug-eluting stents typically have better long-term outcomes but are more expensive.
How can I prevent artery re-narrowing after angioplasty with stent placement?
To prevent re-narrowing, take all prescribed medications (especially blood thinners), maintain a healthy lifestyle with regular exercise, follow a heart-healthy diet, quit smoking, manage underlying conditions, and attend all follow-up appointments with your healthcare provider.