Tension headaches are among the most common types of headaches experienced by adults, affecting millions of people worldwide. These headaches can range from mild discomfort to debilitating pain that interferes with daily activities, work productivity, and overall quality of life.
While occasional tension headaches are typically manageable and not cause for serious concern, understanding their symptoms, triggers, and treatment options can help you better manage this condition and know when professional medical attention may be necessary.
What Is a Tension Headache?
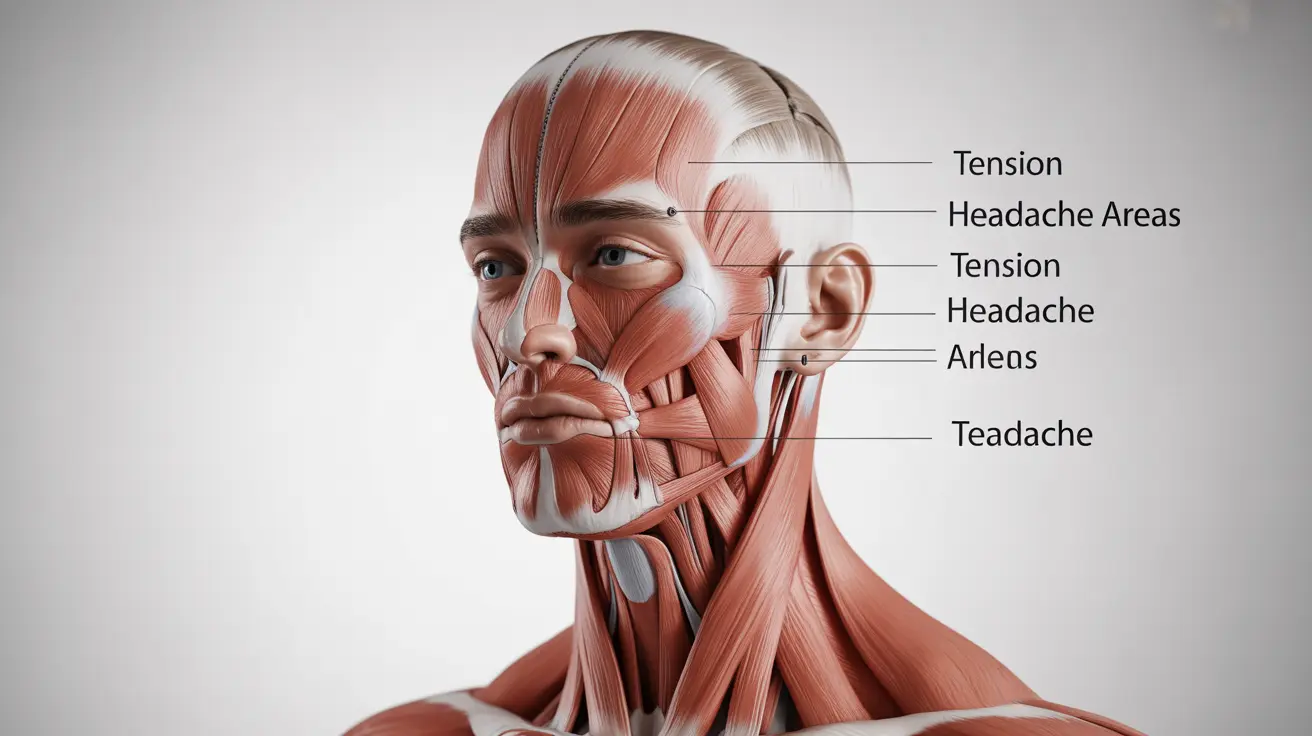
A tension headache is characterized by a steady, aching pain that typically affects both sides of the head. Unlike other headache types, tension headaches create a sensation often described as a tight band or vice-like pressure around the forehead, temples, or back of the head and neck.
These headaches are classified into two main categories: episodic tension headaches, which occur fewer than 15 days per month, and chronic tension headaches, which happen 15 or more days monthly for at least three consecutive months. The pain is usually mild to moderate in intensity and doesn't worsen with routine physical activities.
Common Symptoms and Characteristics
Tension headache symptoms typically develop gradually and can persist for anywhere from 30 minutes to several days. The pain is usually described as dull, pressing, or tightening rather than sharp or throbbing.
Key symptoms include a constant ache on both sides of the head, tenderness in the scalp, neck, and shoulder muscles, and a feeling of pressure or tightness across the forehead or on the sides and back of the head. Unlike migraines, tension headaches rarely cause nausea, vomiting, or sensitivity to light and sound.
How Tension Headaches Differ from Migraines
While both conditions can cause significant discomfort, several key differences distinguish tension headaches from migraines. Tension headaches typically produce bilateral pain that feels like pressure or tightness, whereas migraines often cause unilateral, throbbing pain that may be accompanied by visual disturbances, nausea, and extreme sensitivity to light or sound.
Additionally, tension headaches don't usually worsen with physical activity, while migraine pain often intensifies with movement. Migraines may also be preceded by warning signs called auras, which don't occur with tension headaches.
Primary Causes and Risk Factors
The exact mechanism behind tension headaches isn't fully understood, but research suggests they result from muscle contractions in the head, neck, and shoulder regions. These contractions can be triggered by various physical, emotional, and environmental factors.
Stress is considered one of the most significant triggers, as it causes muscle tension and changes in brain chemistry that can lead to headache development. Poor posture, particularly from prolonged computer use or looking down at mobile devices, can strain neck and shoulder muscles, contributing to tension headache onset.
Sleep and Lifestyle Factors
Inadequate sleep quality or quantity can significantly increase tension headache frequency and intensity. Sleep deprivation affects the body's pain processing mechanisms and increases stress hormone levels, making individuals more susceptible to headache development.
Other lifestyle factors include irregular meal patterns, dehydration, excessive caffeine consumption, eye strain from prolonged screen time, and environmental factors such as bright lights, loud noises, or strong odors.
Effective Treatment and Management Strategies
Most tension headaches respond well to over-the-counter pain medications such as acetaminophen, ibuprofen, or aspirin. However, these should be used according to package directions and not exceed recommended dosages or frequency of use.
Non-medication approaches can be equally effective and include applying heat or cold to the head, neck, or shoulders, gentle massage of the temples, forehead, and neck muscles, and practicing relaxation techniques such as deep breathing or progressive muscle relaxation.
Preventive Lifestyle Modifications
Preventing tension headaches often involves identifying and addressing personal triggers through lifestyle modifications. Maintaining regular sleep schedules, staying adequately hydrated, eating balanced meals at consistent times, and managing stress through exercise, meditation, or other stress-reduction techniques can significantly reduce headache frequency.
Improving posture, especially during work activities, taking regular breaks from computer screens, and ensuring proper ergonomics in workspaces can help prevent muscle strain that contributes to tension headaches.
When to Seek Medical Attention
While most tension headaches can be managed with self-care measures, certain situations warrant professional medical evaluation. Seek immediate medical attention if headaches are sudden and severe, accompanied by fever, stiff neck, confusion, vision changes, or weakness.
Regular medical consultation is recommended if headaches become more frequent or severe, if over-the-counter medications are needed more than twice weekly, or if headaches significantly impact daily activities, work, or sleep patterns.
Diagnostic Process
Healthcare providers typically diagnose tension headaches based on symptom description and physical examination. They may ask about headache patterns, triggers, family history, and current medications. In some cases, additional tests such as CT scans or MRIs may be ordered to rule out other conditions.
Long-term Management and Prevention
Successful long-term management of tension headaches often requires a comprehensive approach combining lifestyle modifications, stress management, and appropriate medical treatment when necessary. Keeping a headache diary can help identify specific triggers and patterns.
Regular exercise, adequate sleep, proper nutrition, and stress reduction techniques form the foundation of effective tension headache prevention. For individuals with frequent tension headaches, healthcare providers may recommend preventive medications or refer to specialists such as neurologists or headache clinics.
Frequently Asked Questions
What are the main symptoms of a tension headache and how does it feel compared to a migraine?
Tension headaches typically cause a steady, pressing, or band-like pain affecting both sides of the head, often described as feeling like a tight cap or vice around the skull. The pain is usually mild to moderate and doesn't worsen with routine activities. In contrast, migraines often cause intense, throbbing pain on one side of the head, accompanied by nausea, vomiting, and sensitivity to light or sound. Migraines may also include visual disturbances or auras, which don't occur with tension headaches.
What lifestyle changes or home remedies can help prevent or relieve tension headaches?
Effective lifestyle changes include maintaining regular sleep schedules, staying hydrated, eating balanced meals at consistent times, managing stress through relaxation techniques, and improving posture during work activities. Home remedies for relief include applying heat or cold packs to the head and neck, gentle massage of temple and neck muscles, practicing deep breathing exercises, ensuring adequate rest in a quiet, dark environment, and taking warm baths or showers to relax tense muscles.
Can poor posture, stress, or lack of sleep really cause tension headaches?
Yes, these factors are well-established triggers for tension headaches. Poor posture, especially from prolonged computer use or looking down at devices, strains neck and shoulder muscles, leading to muscle tension that can trigger headaches. Stress causes both physical muscle tension and changes in brain chemistry that contribute to headache development. Lack of sleep disrupts the body's pain processing mechanisms and increases stress hormone levels, making individuals significantly more susceptible to tension headache occurrence.
When should I see a doctor about my tension headaches, and how are they diagnosed?
Seek medical attention if headaches become more frequent or severe, occur more than twice weekly, significantly impact daily activities, or are accompanied by concerning symptoms like sudden severe onset, fever, stiff neck, vision changes, or weakness. Doctors typically diagnose tension headaches through detailed symptom history, physical examination, and discussion of headache patterns and triggers. Additional tests like CT scans or MRIs may be ordered if other conditions need to be ruled out.
Are over-the-counter painkillers safe for frequent tension headaches, and what are the risks of using them too often?
Over-the-counter medications like acetaminophen, ibuprofen, and aspirin are generally safe when used as directed for occasional tension headaches. However, using these medications more than 2-3 days per week can lead to medication overuse headaches, where the pain medication itself begins causing headaches. Frequent use can also cause stomach problems, liver damage (with acetaminophen), or kidney issues. If you need pain medication more than twice weekly, consult a healthcare provider for alternative treatment strategies and proper headache management.