Breast thermography is gaining attention as a screening method that uses infrared imaging to detect temperature variations in breast tissue. This non-invasive technique measures heat patterns that might indicate early signs of breast abnormalities, including potential cancerous growths. Understanding how thermography works and its role in breast health monitoring can help women make informed decisions about their screening options.
How Breast Thermography Works
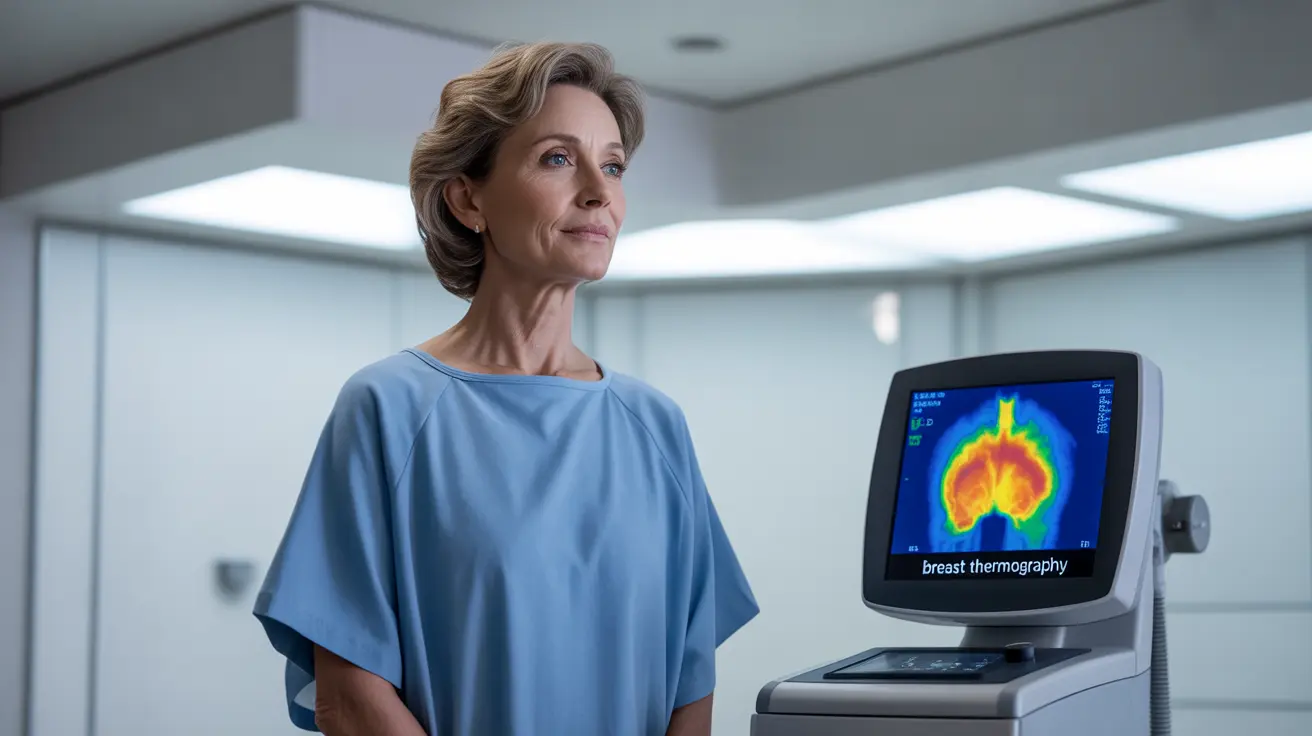
Thermography utilizes sophisticated infrared cameras to create detailed heat maps of breast tissue. The technology is based on the principle that cancer cells have increased metabolic activity and blood flow, creating "hot spots" that can be detected through thermal imaging. These temperature differences may appear before physical changes become noticeable through traditional examination methods.
The Screening Process
During a thermographic examination, patients typically stand in front of a specialized camera in a temperature-controlled room. The procedure is entirely non-contact, and images are taken from various angles to create comprehensive thermal patterns of the breast tissue. The entire process usually takes about 30 minutes and requires no compression or radiation exposure.
Comparing Thermography with Traditional Mammography
While thermography offers certain advantages, it's important to understand its capabilities and limitations compared to mammography, which remains the gold standard for breast cancer screening.
Key Differences
Unlike mammograms, thermography doesn't use radiation or require breast compression. However, it cannot detect physical structures within the breast tissue like mammography can. Instead, it identifies physiological changes that might indicate the presence of cancer or other breast conditions.
Benefits of Breast Thermography
Thermography offers several potential advantages for breast health monitoring:
- Non-invasive and painless procedure
- No radiation exposure
- May detect physiological changes early
- Suitable for all breast types and densities
- Can be used more frequently than mammography
- Particularly useful for younger women with dense breast tissue
Limitations and Considerations
Despite its benefits, thermography has important limitations to consider:
- Not FDA-approved as a standalone screening tool
- May produce false positives or false negatives
- Cannot replace mammography for primary breast cancer screening
- Limited availability and standardization of services
- May not be covered by insurance
Frequently Asked Questions
What is thermography and how does it work for breast cancer screening?
Thermography is an imaging technique that uses infrared technology to detect heat patterns and temperature variations in breast tissue. It works by identifying areas of increased metabolic activity and blood flow that might indicate early signs of cancer development, though it should not be used as a standalone screening method.
Can thermography replace mammography for detecting breast cancer?
No, thermography cannot replace mammography as the primary screening tool for breast cancer. The FDA and medical professionals recommend it only as a complementary method to be used alongside mammography, not as a substitute.
What are the benefits and limitations of using thermography for breast health monitoring?
Benefits include no radiation exposure, non-invasive nature, and potential early detection of physiological changes. Limitations include lower accuracy compared to mammography, lack of standardization, and inability to detect physical structures within the breast tissue.
Is thermography safe and does it involve radiation exposure?
Yes, thermography is completely safe and involves no radiation exposure. It's a non-invasive procedure that only measures the natural heat emissions from your body using infrared imaging technology.
How accurate is thermography compared to a mammogram in detecting breast cancer?
Thermography is generally less accurate than mammography in detecting breast cancer. While it may detect physiological changes early, it has higher rates of both false positives and false negatives compared to mammography. This is why it's recommended as a complementary tool rather than a primary screening method.