Uterine atony is a serious postpartum complication that occurs when the uterus fails to contract effectively after childbirth. This condition requires immediate medical attention as it can lead to excessive bleeding and potentially life-threatening complications. Understanding the signs, risk factors, and treatment options is crucial for both healthcare providers and expectant mothers.
This comprehensive guide explores everything you need to know about uterine atony, from its early warning signs to the latest treatment approaches and preventive measures.
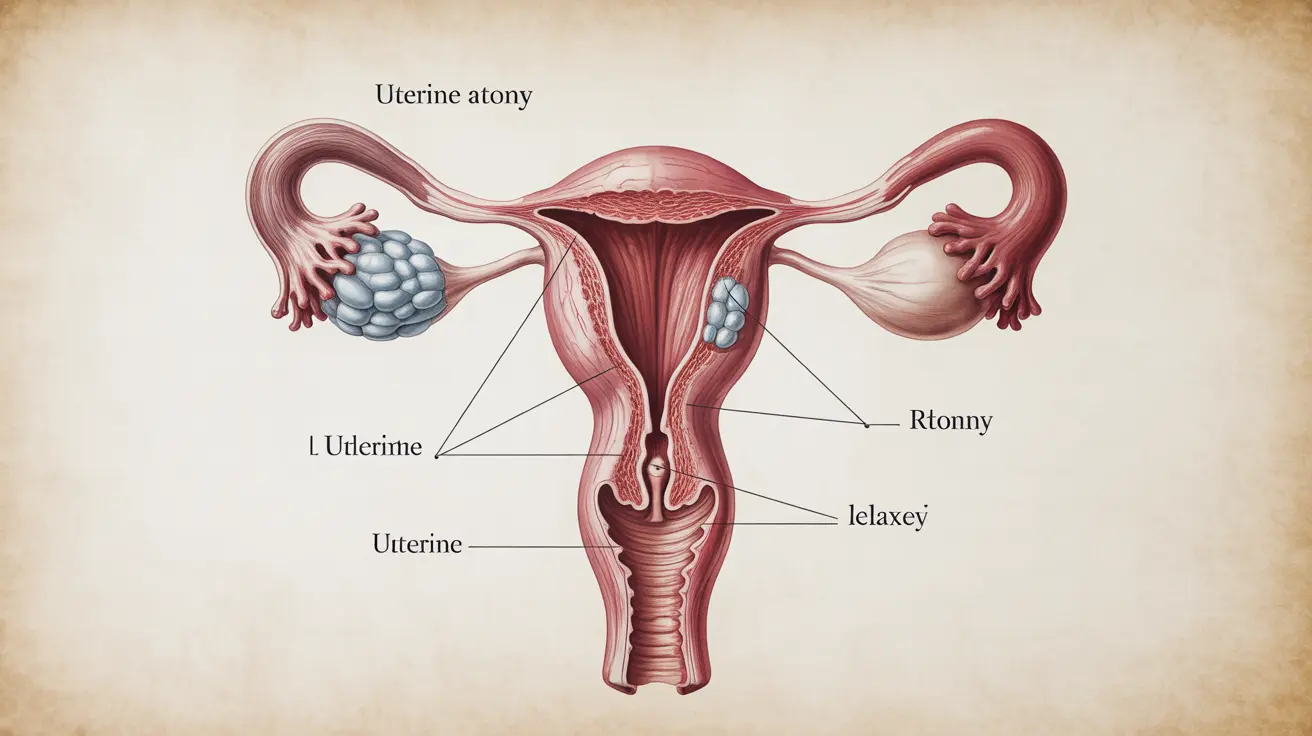
What is Uterine Atony?
Uterine atony occurs when the uterine muscles lose their ability to contract properly following delivery. These contractions are essential for preventing excessive blood loss and helping the uterus return to its pre-pregnancy size. When the uterus remains relaxed instead of contracting, it can result in severe postpartum hemorrhage.
Recognizing the Signs and Symptoms
Early recognition of uterine atony symptoms is crucial for prompt intervention. The most common indicators include:
- Excessive vaginal bleeding after delivery
- A soft or "boggy" feeling uterus upon physical examination
- Lower abdominal pain or discomfort
- Signs of shock (rapid heart rate, low blood pressure, dizziness)
- Pale skin and cold sweats
Risk Factors and Prevention
Several factors can increase the likelihood of developing uterine atony:
- Multiple pregnancies or previous multiple births
- Prolonged labor
- Overdistended uterus
- History of previous uterine atony
- Advanced maternal age
- Placental abnormalities
- Use of certain medications during labor
Diagnostic Approach
Healthcare providers diagnose uterine atony through:
- Physical examination of the uterus
- Assessment of blood loss
- Vital sign monitoring
- Ultrasound imaging when necessary
- Laboratory tests to check blood counts and clotting factors
Treatment Methods
Medical Management
Initial treatment typically involves medication-based approaches:
- Uterotonic medications to stimulate contractions
- IV fluid administration
- Blood product transfusions when necessary
- Careful monitoring of vital signs
Surgical Interventions
In cases where medical management isn't sufficient, surgical options may include:
- Uterine compression sutures
- Uterine artery ligation
- Hysterectomy in severe cases
Prevention Strategies
Healthcare providers implement several preventive measures during labor and delivery:
- Active management of the third stage of labor
- Early identification of risk factors
- Proper oxytocin administration
- Regular monitoring of uterine tone
- Preparation of emergency protocols
Frequently Asked Questions
What are the main symptoms indicating uterine atony after childbirth?
The primary symptoms include heavy vaginal bleeding that doesn't slow down, a soft or relaxed uterus upon examination, and signs of blood loss such as dizziness, rapid heartbeat, and low blood pressure.
How is uterine atony diagnosed by healthcare providers?
Healthcare providers diagnose uterine atony through physical examination of the uterus, assessment of blood loss volume, monitoring vital signs, and sometimes using ultrasound imaging to confirm the diagnosis.
What treatments are used to manage uterine atony and stop postpartum bleeding?
Treatment involves a combination of uterotonic medications, uterine massage, IV fluids, and blood products if necessary. In severe cases, surgical interventions may be required, including compression sutures or, rarely, hysterectomy.
What are the common risk factors that increase the likelihood of uterine atony?
Common risk factors include multiple pregnancies, prolonged labor, overdistended uterus, previous uterine atony, advanced maternal age, and certain placental conditions.
How can uterine atony be prevented or prepared for during labor and delivery?
Prevention strategies include active management of the third stage of labor, early risk assessment, appropriate use of oxytocin, continuous monitoring of uterine tone, and having emergency protocols in place.