Vaginismus is a complex but treatable condition that causes involuntary muscle spasms in the vaginal area, making penetration difficult or impossible. This condition can significantly impact intimate relationships, medical examinations, and overall quality of life. Understanding its causes, symptoms, and available treatments is crucial for those affected and their partners.
While the exact prevalence of vaginismus isn't fully known, it affects women of all ages and backgrounds. The good news is that with proper diagnosis and treatment, most women can overcome this condition and achieve comfortable penetration.
Understanding Vaginismus and Its Impact
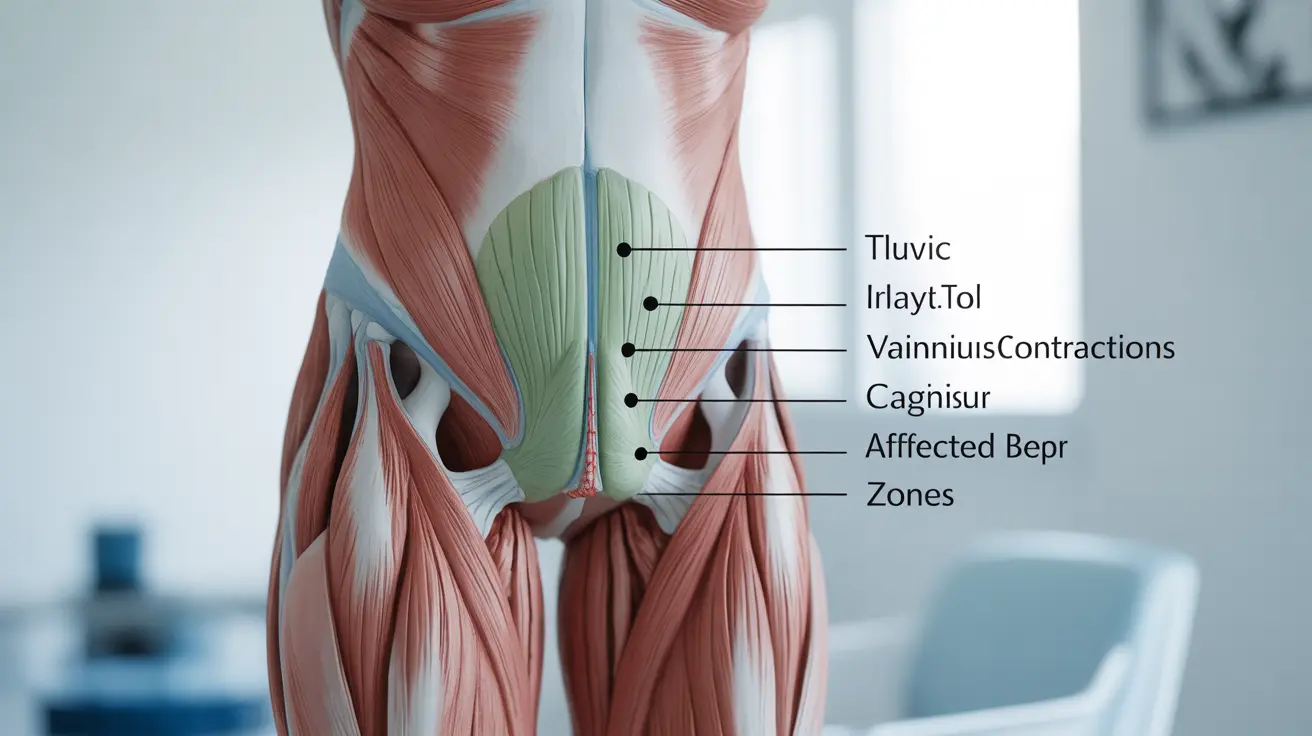
Vaginismus involves the involuntary contraction of pelvic floor muscles surrounding the vagina. These contractions can occur when any form of penetration is attempted, whether during sexual activity, tampon insertion, or medical examinations. The severity can vary from mild discomfort to complete inability to achieve penetration.
The condition can be primary (present from the first attempt at penetration) or secondary (developing after a period of normal sexual function). Both types require different approaches to treatment and understanding.
Common Signs and Symptoms
The manifestation of vaginismus can vary among individuals, but common symptoms include:
- Burning or stinging sensation during attempted penetration
- Intense fear or anxiety about penetration
- Involuntary muscle tightening in the pelvic area
- Difficulty with gynecological examinations
- Pain or discomfort when inserting tampons
- Emotional distress related to intimate activities
Understanding the Causes
Vaginismus can develop due to various factors, often involving both physical and psychological components:
Physical Factors
- Previous painful experiences during penetration
- Childbirth trauma
- Infections or medical conditions
- Hormonal changes
- Pelvic floor dysfunction
Psychological Factors
- Past traumatic experiences
- Religious or cultural beliefs about sexuality
- Relationship issues
- General anxiety or stress
- Fear of pain during intercourse
Diagnosis and Medical Assessment
Healthcare providers typically diagnose vaginismus through a combination of medical history review, discussion of symptoms, and gentle physical examination when possible. The diagnosis process is conducted with sensitivity and at the patient's comfort level.
Treatment Approaches
Physical Therapy
Physical therapy often plays a crucial role in treatment, including:
- Pelvic floor exercises
- Relaxation techniques
- Progressive dilator therapy
- Biofeedback training
Psychological Support
Many patients benefit from psychological interventions such as:
- Cognitive behavioral therapy (CBT)
- Anxiety management techniques
- Couples counseling when appropriate
- Exposure therapy
Medical Interventions
Additional medical treatments may include:
- Topical medications for pain management
- Botox injections in some cases
- Muscle relaxants when appropriate
- Treatment of underlying conditions
Frequently Asked Questions
What are the most common symptoms of vaginismus and how can I tell if I have it?
The most common symptoms include involuntary muscle spasms during attempted penetration, burning or stinging sensations, and anxiety about penetration. If you experience these symptoms consistently, consult a healthcare provider for proper diagnosis.
What causes vaginismus and are anxiety or past trauma linked to this condition?
Vaginismus can be caused by both physical and psychological factors. Anxiety and past trauma are indeed common contributors, along with physical factors like injuries, infections, or hormonal changes.
How is vaginismus diagnosed by healthcare providers, and what should I expect during a pelvic exam?
Diagnosis typically involves a detailed medical history and gentle physical examination. Healthcare providers will work at your comfort level, and you can stop the examination at any time. The exam focuses on identifying muscle tension and ruling out other conditions.
What are the most effective treatment options for vaginismus, including physical and psychological therapies?
The most effective treatments often combine physical therapy (including dilator therapy and pelvic floor exercises) with psychological support like CBT. Treatment plans are customized to each individual's needs and circumstances.
How long does vaginismus treatment usually take, and is it possible to resume pain-free sexual activity?
Treatment duration varies by individual, typically ranging from a few months to a year. With proper treatment and patience, most women can achieve pain-free penetration and resume normal sexual activity.