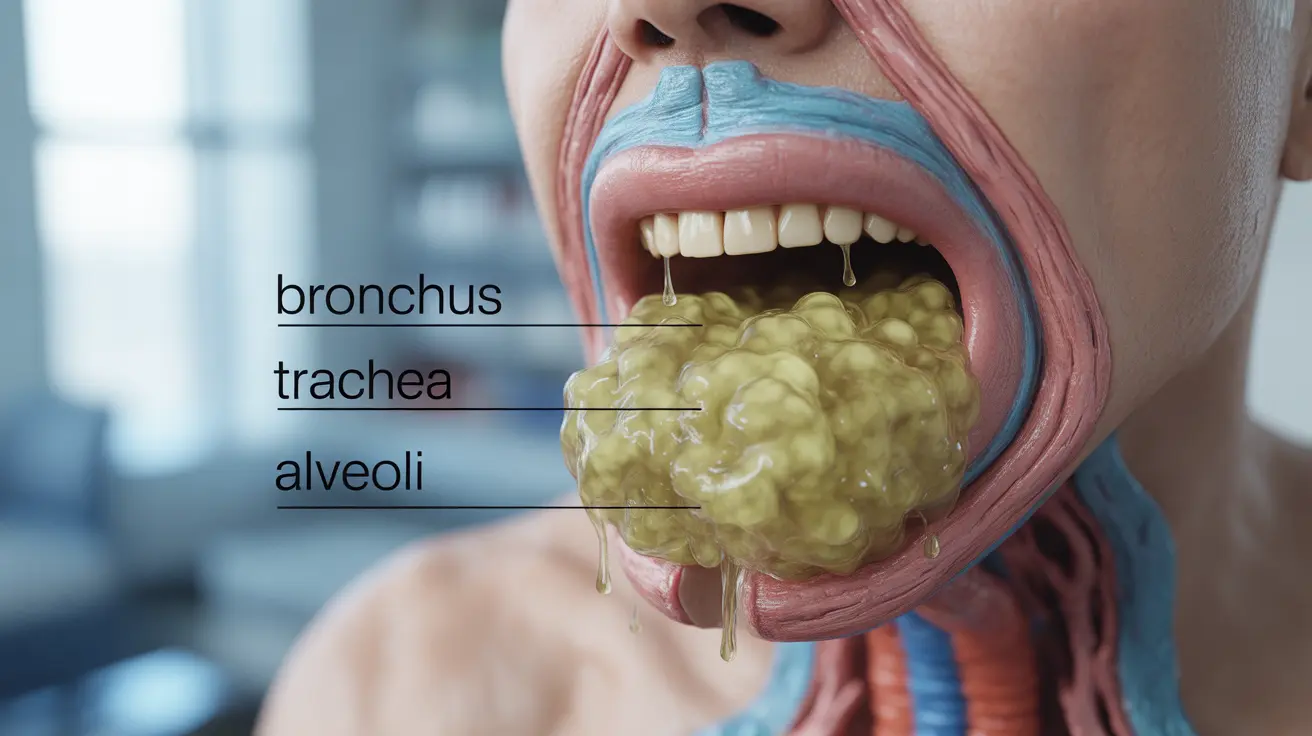
A wet cough, also known as a productive cough, occurs when your airways produce excess mucus as part of your body's natural defense mechanism against illness. Understanding the nature of a wet cough, its causes, and proper management strategies is crucial for effective treatment and knowing when to seek medical attention.
Unlike its dry counterpart, a wet cough serves an important purpose: clearing airways of mucus and potential pathogens. However, persistent wet coughs can signal underlying health conditions that may require medical intervention.
Understanding Wet Coughs and Their Causes
Wet coughs typically develop due to various respiratory conditions that trigger increased mucus production. Common causes include:
- Bacterial or viral infections
- Bronchitis
- Pneumonia
- Chronic conditions like COPD
- Postnasal drip
- Bronchiectasis
The presence of mucus in a wet cough often indicates that your body is actively fighting an infection or responding to irritation in the airways. The color and consistency of the mucus can provide important clues about the underlying cause.
Distinguishing Features of a Wet Cough
A wet cough has several characteristic features that set it apart from other types of coughs:
Physical Characteristics
- Feels "loose" in the chest
- Produces visible mucus when coughing
- Often accompanied by a gurgling sensation
- May worsen in the morning
Associated Symptoms
Depending on the underlying cause, a wet cough may be accompanied by:
- Fever
- Chest congestion
- Fatigue
- Shortness of breath
- Wheezing
Effective Treatment Approaches
Treatment for a wet cough varies depending on its cause and severity. Several approaches can help manage symptoms and promote recovery:
Home Remedies
- Stay hydrated to thin mucus
- Use a humidifier
- Try honey and warm liquids
- Practice good sleep positioning
- Keep the air clean and free from irritants
Medical Treatments
When home remedies aren't sufficient, medical interventions may include:
- Expectorants to help loosen mucus
- Prescription medications for underlying conditions
- Antibiotics (only when bacterial infection is confirmed)
- Inhaled medications for certain respiratory conditions
When to Seek Medical Attention
While many wet coughs resolve with home care, certain symptoms warrant professional medical evaluation:
- Cough lasting more than 3 weeks
- Difficulty breathing
- High fever
- Blood in mucus
- Chest pain
- Significant fatigue or weakness
Frequently Asked Questions
What are the common causes of a wet cough and how can I tell if mine is serious? A wet cough is commonly caused by respiratory infections, bronchitis, or chronic conditions like COPD. It's serious if accompanied by high fever, difficulty breathing, chest pain, or if it persists beyond three weeks.
How is a wet cough different from a dry cough, and why does it produce mucus? A wet cough produces mucus as part of the body's defense mechanism to clear airways of infections or irritants. Dry coughs, in contrast, don't produce mucus and are typically triggered by throat irritation or inflammation.
What are effective home remedies and treatments for relieving a wet cough? Effective home remedies include staying well-hydrated, using a humidifier, taking honey, practicing good sleep positioning, and avoiding irritants. Over-the-counter expectorants can also help loosen mucus.
When should I see a doctor for a wet cough and what symptoms indicate urgent medical attention? Seek medical attention if your wet cough persists beyond three weeks, produces blood-tinged mucus, causes breathing difficulties, or is accompanied by high fever or severe chest pain.
Are antibiotics necessary for treating a wet cough caused by respiratory infections? Antibiotics are only necessary when a bacterial infection is confirmed as the cause of the wet cough. Most respiratory infections are viral and won't respond to antibiotics, making them unnecessary in many cases.