A hysterectomy is often a primary treatment option for uterine cancer, and understanding the outlook after this procedure is crucial for patients and their families. The prognosis after a hysterectomy for uterine cancer can vary significantly based on several factors, including the cancer stage at diagnosis and the specific treatment approach used.
Factors Affecting Survival Rates
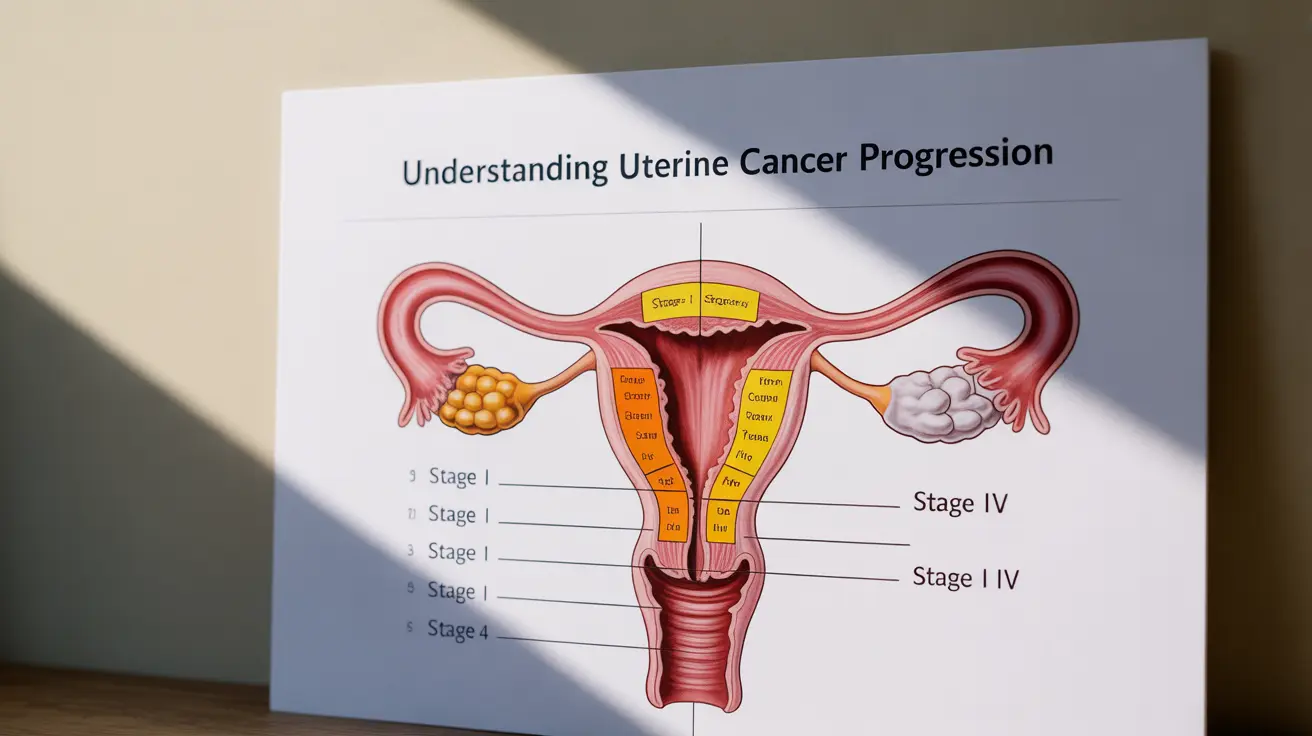
The prognosis following a hysterectomy for uterine cancer largely depends on how early the cancer was detected and treated. Early-stage uterine cancers typically have more favorable outcomes, with five-year survival rates reaching up to 95% for Stage I cancers. As the stage increases, these rates may decrease, highlighting the importance of early detection and prompt treatment.
Impact of Cancer Stage
- Stage I: Cancer confined to the uterus
- Stage II: Cancer has spread to the cervix
- Stage III: Cancer has spread to nearby tissues or lymph nodes
- Stage IV: Cancer has spread to distant organs
Recovery and Follow-up Care
- Initial hospital stay: 2-3 days for minimally invasive procedures
- Basic activity resumption: 3-4 weeks
- Full recovery: 6-8 weeks
Regular follow-up care is essential and typically includes:
- Frequent check-ups in the first year
- Physical examinations
- Imaging tests as needed
- Blood tests to monitor for potential recurrence
Additional Treatment Considerations
While a hysterectomy is often the primary treatment, additional therapies may be recommended to improve outcomes:
- Radiation therapy
- Chemotherapy
- Hormone therapy
- Targeted therapy
These treatments may be used before or after surgery, depending on individual circumstances and cancer characteristics.
Risk of Recurrence
- Initial cancer stage
- Grade of the tumor
- Completeness of surgical removal
- Response to additional treatments
Regular monitoring and prompt attention to any new symptoms are crucial for early detection of potential recurrence.
Frequently Asked Questions
What is the typical prognosis for uterine cancer after a hysterectomy?
The typical prognosis varies by stage but is generally favorable for early-stage cancers, with five-year survival rates above 90% for Stage I cases. Later stages may have lower survival rates but can still respond well to comprehensive treatment.How does the stage of uterine cancer at diagnosis affect survival after hysterectomy?
Cancer stage significantly impacts survival rates. Early-stage cancers confined to the uterus have the best prognosis, while advanced stages with spread to other organs have lower survival rates.What are the chances of uterine cancer coming back after a hysterectomy?
Recurrence risks vary based on cancer stage, grade, and other factors. Early-stage cancers have lower recurrence rates, typically less than 10%, while advanced stages may have higher risks.How long is recovery after a hysterectomy for uterine cancer, and what follow-up care is needed?
Most patients recover within 6-8 weeks. Follow-up care includes regular check-ups, physical exams, and monitoring tests for at least five years after surgery.Can additional treatments like radiation or chemotherapy improve outcomes after hysterectomy for uterine cancer?
Yes, additional treatments can significantly improve outcomes, especially for higher-risk cases. These therapies may help reduce recurrence risks and improve survival rates when used appropriately.