Learning about uterine cancer survival rates can provide valuable insights for patients and their loved ones. While statistics can seem daunting, understanding these numbers helps create a clearer picture of what to expect and highlights the importance of early detection and proper treatment.
This comprehensive guide explores the various factors that influence uterine cancer survival rates, including cancer stage, type, and other important considerations that can impact prognosis.
Overall Survival Rates for Uterine Cancer
The general outlook for uterine cancer is relatively positive compared to many other cancers, particularly when detected early. The overall five-year survival rate for uterine cancer varies significantly based on the stage at diagnosis and other factors.
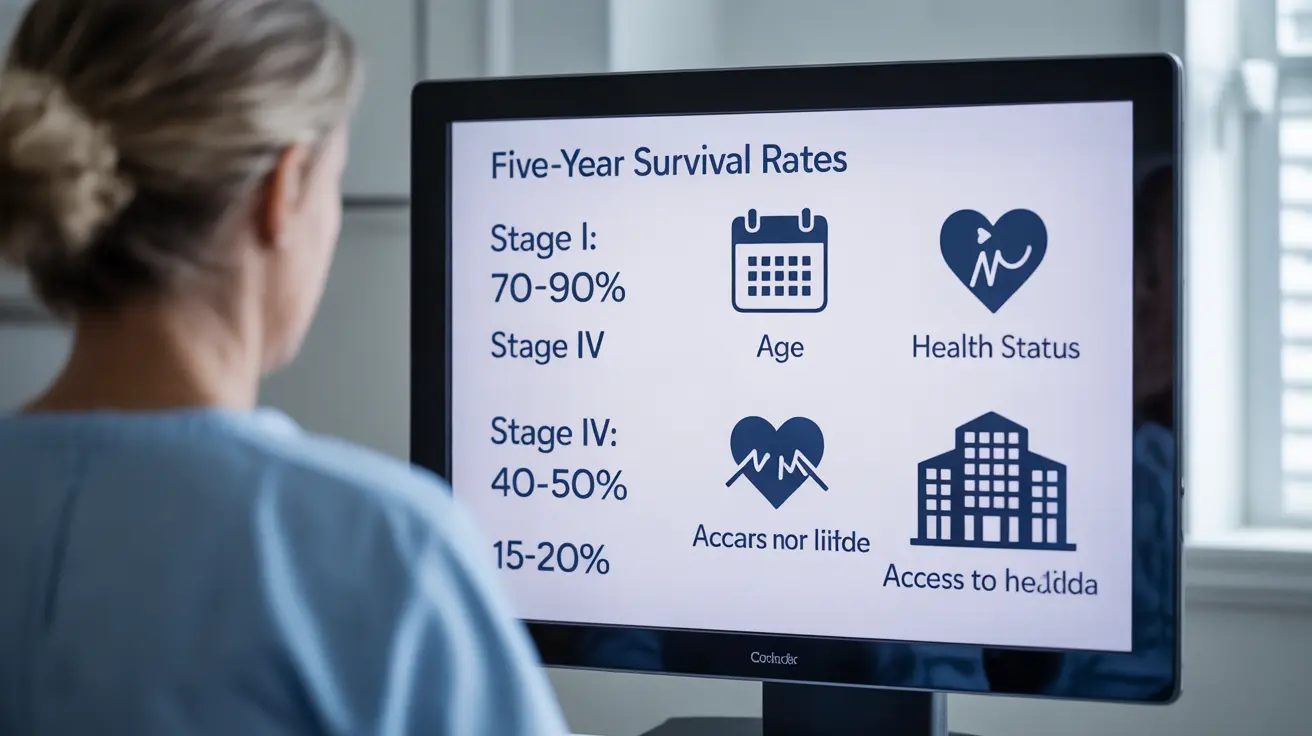
Stage-Based Survival Rates
- Stage I: Approximately 90% five-year survival rate
- Stage II: Around 70% five-year survival rate
- Stage III: About 40-50% five-year survival rate
- Stage IV: Roughly 15-20% five-year survival rate
Types of Uterine Cancer and Their Impact on Survival
Different types of uterine cancer can significantly affect survival rates:
Endometrial Adenocarcinoma
This most common type of uterine cancer typically has better survival rates, especially when detected early. Type 1 endometrial cancers generally have a more favorable prognosis than Type 2.
Uterine Sarcoma
This less common but more aggressive form typically has lower survival rates due to its tendency to spread more quickly and respond differently to standard treatments.
Key Factors Affecting Survival Rates
Several factors can influence survival outcomes:
- Age at diagnosis
- Overall health status
- Response to treatment
- Access to healthcare
- Genetic factors
- Presence of other medical conditions
The Critical Role of Early Detection
Early detection significantly improves survival rates for uterine cancer. Regular check-ups and prompt attention to symptoms such as abnormal bleeding can lead to earlier diagnosis and better outcomes.
Warning Signs to Watch For
- Postmenopausal bleeding
- Irregular menstrual periods
- Pelvic pain or pressure
- Unexplained weight loss
- Difficulty urinating
Racial Disparities in Survival Rates
Research has shown significant disparities in uterine cancer survival rates among different racial groups. Black women, in particular, often face lower survival rates due to various factors including:
- Later stage at diagnosis
- Limited access to healthcare
- Different tumor characteristics
- Socioeconomic barriers to treatment
Frequently Asked Questions
What is the five-year survival rate for uterine cancer at different stages?
The five-year survival rate varies significantly by stage: Stage I has about 90% survival rate, Stage II around 70%, Stage III approximately 40-50%, and Stage IV roughly 15-20%. These rates are general statistics and individual outcomes may vary.
How does the type of uterine cancer affect survival rates?
Endometrial adenocarcinoma typically has better survival rates than uterine sarcoma. Type 1 endometrial cancers generally have more favorable outcomes than Type 2, while uterine sarcomas tend to have lower survival rates due to their aggressive nature.
What factors influence the survival chances of someone diagnosed with uterine cancer?
Key factors include cancer stage at diagnosis, cancer type, age, overall health status, access to healthcare, genetic factors, and presence of other medical conditions. The response to treatment also plays a crucial role in survival outcomes.
Why is early detection important for improving uterine cancer survival rates?
Early detection allows for treatment before the cancer spreads, significantly improving survival rates. When caught in Stage I, survival rates can be as high as 90%, compared to much lower rates in advanced stages.
Are there differences in uterine cancer survival rates between different racial groups?
Yes, significant disparities exist. Black women typically have lower survival rates due to factors including later-stage diagnosis, limited healthcare access, different tumor characteristics, and socioeconomic barriers to treatment.