When it comes to vein problems in the legs, distinguishing between varicose veins and deep vein thrombosis (DVT) is crucial for proper treatment and preventing potentially serious complications. While both conditions affect the blood vessels in your legs, they have distinct characteristics, causes, and levels of medical urgency.
This comprehensive guide will help you understand the key differences between these two vascular conditions, their symptoms, risk factors, and treatment approaches. Knowing these distinctions could potentially save your life, as DVT requires immediate medical attention while varicose veins typically don't pose an immediate health threat.
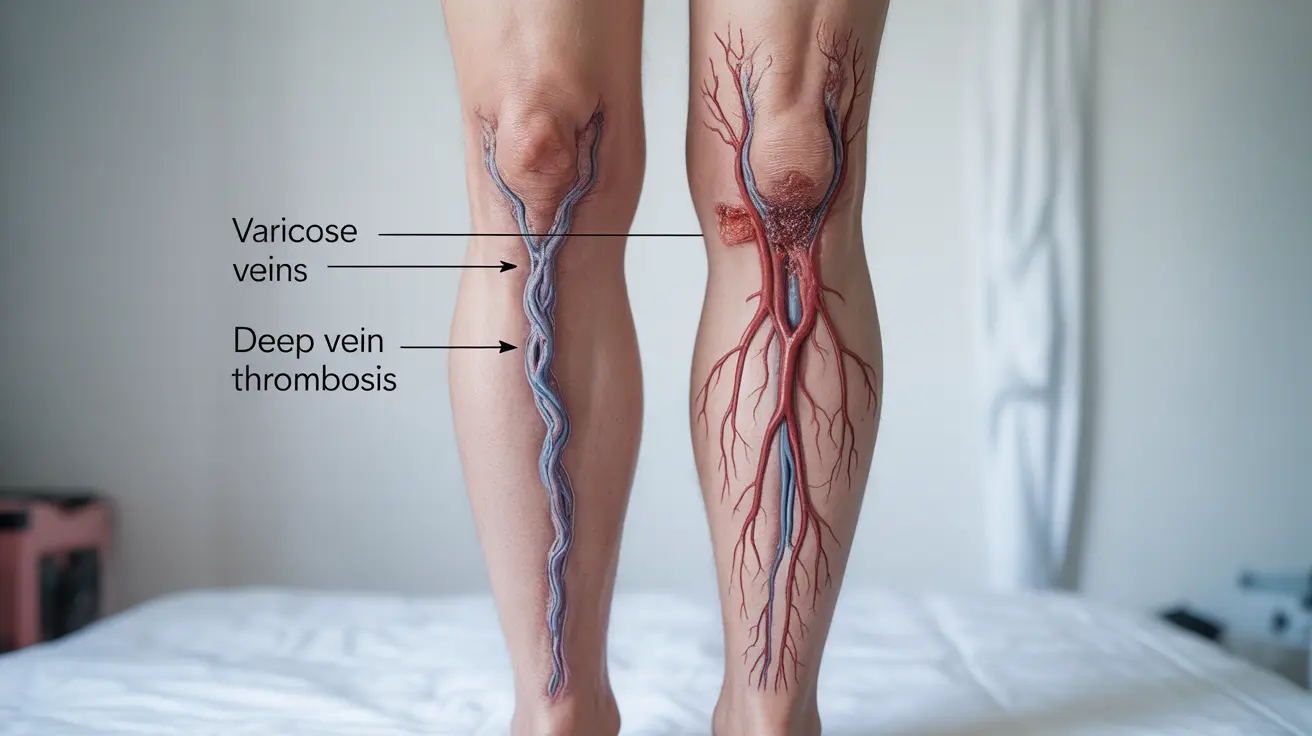
Understanding Varicose Veins and DVT
Varicose veins are enlarged, twisted superficial veins that typically appear just beneath the skin's surface. They occur when vein valves malfunction, allowing blood to pool instead of flowing efficiently back to the heart. While often cosmetically concerning, they're usually not dangerous.
Deep vein thrombosis, on the other hand, occurs when a blood clot forms in one of the deep veins, typically in the legs. This condition is more serious and requires immediate medical attention, as blood clots can break loose and travel to the lungs, causing a potentially life-threatening pulmonary embolism.
Key Physical Differences and Symptoms
Varicose Vein Characteristics
- Visible twisted, rope-like veins
- Blue or purple in color
- Located close to the skin's surface
- Often cause aching or heavy legs
- May cause itching or burning sensation
- Symptoms typically worse at day's end
DVT Characteristics
- Often not visible on the surface
- Sudden leg pain or tenderness
- Significant swelling in one leg
- Warm skin over the affected area
- Redness or discoloration
- Symptoms can develop rapidly
Risk Factors and Prevention
Varicose Vein Risk Factors
- Age (risk increases with age)
- Family history
- Pregnancy
- Obesity
- Standing or sitting for long periods
- Female gender
DVT Risk Factors
- Recent surgery or hospitalization
- Cancer
- Long periods of immobility
- Trauma or injury
- Hormone therapy or birth control
- Smoking
- Obesity
Treatment Approaches
Managing Varicose Veins
- Compression stockings
- Exercise and weight management
- Elevation of legs
- Sclerotherapy
- Laser treatment
- Radiofrequency ablation
- Vein stripping (in severe cases)
Treating DVT
- Blood thinners (anticoagulants)
- Immediate medical intervention
- Possible hospitalization
- IVC filters in some cases
- Clot-busting medications
- Regular monitoring and follow-up
Frequently Asked Questions
What are the main differences in symptoms between varicose veins and deep vein thrombosis (DVT)? Varicose veins typically present as visible, twisted veins with mild discomfort, while DVT often shows no visible surface changes but causes sudden, severe pain, swelling, and warmth in one leg.
How can I tell if leg pain and swelling are caused by varicose veins or a serious condition like DVT? Varicose vein pain tends to be chronic and mild, worsening throughout the day. DVT pain is usually sudden, severe, and accompanied by significant swelling in one leg. If you suspect DVT, seek immediate medical attention.
What risk factors increase the chances of developing varicose veins versus DVT? Varicose veins are mainly influenced by age, genetics, pregnancy, and prolonged standing. DVT risk factors include recent surgery, immobility, cancer, and blood-clotting disorders.
What treatment options are available for varicose veins compared to deep vein thrombosis? Varicose veins can be treated with conservative measures like compression stockings or procedures like sclerotherapy. DVT requires immediate medical intervention with blood thinners and possible hospitalization.
Can having varicose veins increase my risk of getting deep vein thrombosis? While varicose veins alone don't directly cause DVT, they can indicate underlying venous insufficiency, which may increase DVT risk. Regular monitoring and proper management of varicose veins can help reduce potential complications.