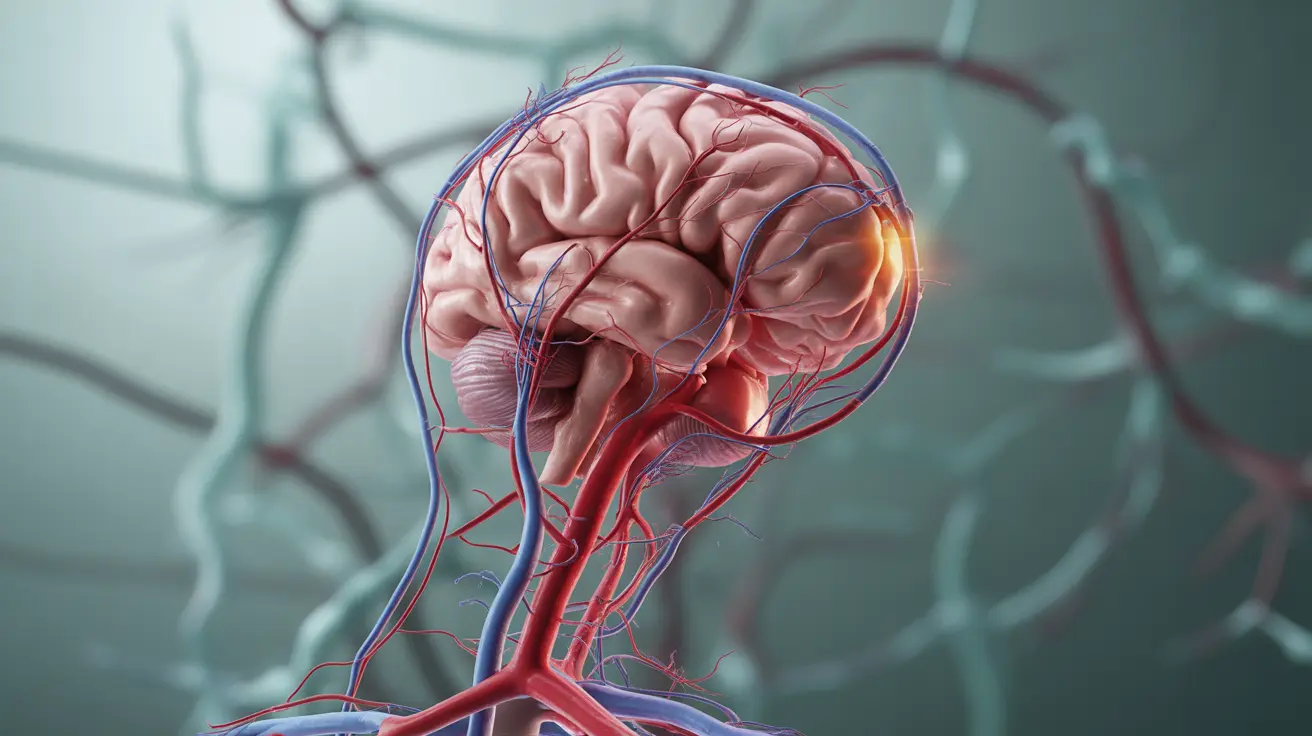
Vertebrobasilar insufficiency (VBI) is a serious circulatory condition that affects blood flow to the back of the brain through the vertebral and basilar arteries. This reduced blood supply can lead to various neurological symptoms and potentially increase the risk of stroke. Understanding its symptoms, causes, and treatment options is crucial for effective management and prevention.
This comprehensive guide will explore the key aspects of vertebrobasilar insufficiency, helping you recognize its signs, understand its implications, and learn about available treatment approaches.
Recognizing the Signs and Symptoms
Vertebrobasilar insufficiency can manifest through various symptoms that may significantly impact daily life. Common indicators include:
- Dizziness and vertigo
- Visual disturbances or temporary vision loss
- Balance problems and unsteady gait
- Difficulty speaking or slurred speech
- Headaches, particularly in the back of the head
- Numbness or weakness in the limbs
- Coordination problems
These symptoms often occur suddenly and may be temporary, lasting from a few minutes to several hours. Some people experience them more frequently when changing head positions or during specific movements.
Understanding the Causes and Risk Factors
Several factors can contribute to the development of vertebrobasilar insufficiency:
Primary Causes
- Atherosclerosis (hardening of arteries)
- Cervical spine disorders
- Blood clots
- Arterial dissection
Risk Factors
- Advanced age
- High blood pressure
- Diabetes
- Smoking
- High cholesterol
- Obesity
- Sedentary lifestyle
Diagnostic Approaches
Healthcare providers use various methods to diagnose vertebrobasilar insufficiency accurately:
Physical Examination
Doctors perform detailed neurological examinations and assess symptoms during different head positions and movements.
Imaging Tests
- Magnetic Resonance Imaging (MRI)
- Magnetic Resonance Angiography (MRA)
- Computed Tomography (CT) scan
- Doppler ultrasound
Treatment Options and Management
Treatment for vertebrobasilar insufficiency typically involves a multi-faceted approach:
Medical Interventions
- Antiplatelet medications
- Blood pressure management
- Cholesterol-lowering drugs
- Blood thinners when appropriate
Lifestyle Modifications
- Regular exercise programs
- Smoking cessation
- Dietary changes
- Weight management
- Stress reduction techniques
Prevention Strategies
Taking proactive steps to prevent vertebrobasilar insufficiency and its complications is essential:
- Regular blood pressure monitoring
- Maintaining healthy cholesterol levels
- Regular physical activity
- Balanced nutrition
- Regular medical check-ups
- Avoiding tobacco products
Frequently Asked Questions
What are the common symptoms of vertebrobasilar insufficiency and how do they affect daily life? Symptoms include dizziness, vertigo, visual problems, balance issues, and difficulty speaking. These symptoms can significantly impact daily activities, making tasks like driving, walking, or reading challenging.
What causes vertebrobasilar insufficiency and which risk factors increase the likelihood of developing it? The main causes include atherosclerosis, cervical spine disorders, and blood clots. Risk factors include advanced age, high blood pressure, diabetes, smoking, and high cholesterol.
How is vertebrobasilar insufficiency diagnosed and what tests are typically used? Diagnosis involves a combination of physical examination, neurological assessment, and imaging tests such as MRI, MRA, CT scans, and Doppler ultrasound studies.
What treatment options are available for vertebrobasilar insufficiency and how can lifestyle changes help? Treatment options include medications like antiplatelets and blood thinners, along with lifestyle modifications such as exercise, dietary changes, and stress management techniques.
How can vertebrobasilar insufficiency be prevented and what steps reduce the risk of stroke? Prevention focuses on controlling risk factors through regular exercise, healthy diet, blood pressure management, cholesterol control, and avoiding tobacco use. Regular medical check-ups are also essential for early detection and management.