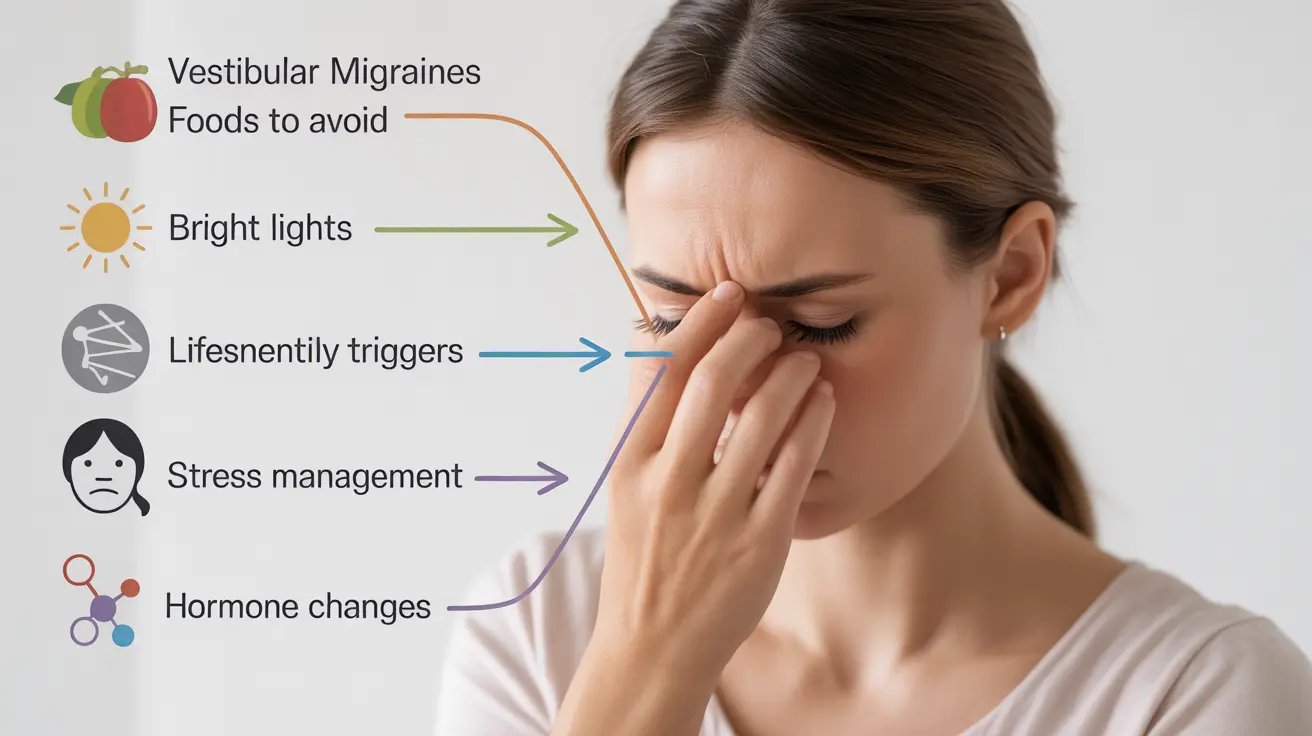
Living with vestibular migraines can be challenging, as these unique headaches combine traditional migraine symptoms with distinct balance and dizziness issues. Understanding what triggers these episodes is crucial for effective management and prevention. This guide explores the most common vestibular migraine triggers and provides practical strategies for identifying and managing them.
Common Triggers of Vestibular Migraines
Vestibular migraines can be triggered by various factors, and identifying these triggers is essential for developing an effective management strategy. Understanding your personal triggers can help reduce the frequency and severity of episodes.
Dietary Factors
Many people with vestibular migraines find that certain foods and beverages can trigger episodes. Common dietary triggers include:
- Aged cheeses and fermented foods
- Processed meats containing nitrates
- Caffeine and alcohol
- MSG and artificial sweeteners
- Foods high in tyramine
Keeping a detailed food diary can help identify specific dietary triggers that affect you personally. Track what you eat and when symptoms occur to establish patterns and connections.
Environmental Triggers
Environmental factors can significantly impact vestibular migraine occurrence. Key environmental triggers include:
- Bright or flickering lights
- Sudden changes in barometric pressure
- Strong odors or perfumes
- Loud noises or certain sound patterns
- Temperature extremes
Lifestyle and Physical Triggers
Daily activities and lifestyle factors can play a crucial role in triggering vestibular migraines. Understanding these triggers can help in developing preventive strategies.
Stress and Sleep Patterns
Stress management and maintaining healthy sleep habits are crucial for preventing vestibular migraines. Common stress-related triggers include:
- Emotional stress and anxiety
- Poor sleep quality
- Irregular sleep schedules
- Physical exhaustion
- Work-related stress
Motion and Physical Activities
Certain types of movement and physical activities can trigger episodes:
- Rapid head movements
- Screen time and digital device use
- Car rides or travel motion
- Exercise (especially high-impact activities)
- Visual stimulation from patterns or movement
Hormonal Influences
Hormonal changes can significantly affect vestibular migraine patterns, particularly in women. Key hormonal triggers include:
- Menstrual cycle fluctuations
- Pregnancy and postpartum changes
- Perimenopause and menopause
- Hormonal medication changes
- Birth control use or discontinuation
Frequently Asked Questions
What are the most common triggers that cause vestibular migraine episodes?
The most common triggers include dietary factors (such as certain foods and beverages), environmental changes (like weather and bright lights), stress, sleep disturbances, hormonal fluctuations, and specific physical activities or movements.
How can I identify and avoid food triggers that worsen vestibular migraines?
Keep a detailed food diary to track what you eat and when symptoms occur. Common food triggers include aged cheese, processed meats, caffeine, and alcohol. Once identified, gradually eliminate suspected trigger foods and note any improvement in symptoms.
What lifestyle changes can help prevent vestibular migraines related to stress and sleep disturbances?
Establish a regular sleep schedule, practice stress-reduction techniques like meditation or yoga, maintain consistent exercise routines, and implement relaxation practices. Creating a calm bedroom environment and avoiding screens before bedtime can also help.
How do hormonal changes affect the frequency or severity of vestibular migraines?
Hormonal fluctuations, particularly during menstrual cycles, pregnancy, and menopause, can influence vestibular migraine patterns. Working with healthcare providers to manage hormonal changes and tracking symptoms throughout your cycle can help identify patterns and develop appropriate management strategies.
Can weather and light exposure trigger vestibular migraines, and how can I manage these environmental factors?
Yes, weather changes and light exposure can trigger episodes. Monitor weather forecasts to prepare for barometric pressure changes, use FL-41 tinted glasses for light sensitivity, and create controlled environments when possible. Avoiding bright or flickering lights and using proper lighting at home and work can help minimize triggers.