The ability to void urine is a fundamental bodily function that most people take for granted until problems arise. Urinary voiding, the medical term for releasing urine from the bladder, involves a complex coordination between the nervous system, bladder muscles, and urethral sphincters. When this process works smoothly, it happens almost automatically, but various conditions can disrupt normal voiding patterns.
Understanding how urination works and recognizing signs of voiding dysfunction can help you maintain better urinary health and seek appropriate medical care when needed. This comprehensive guide explores the normal voiding process, common symptoms of dysfunction, and available treatment options.
The Normal Urinary Voiding Process
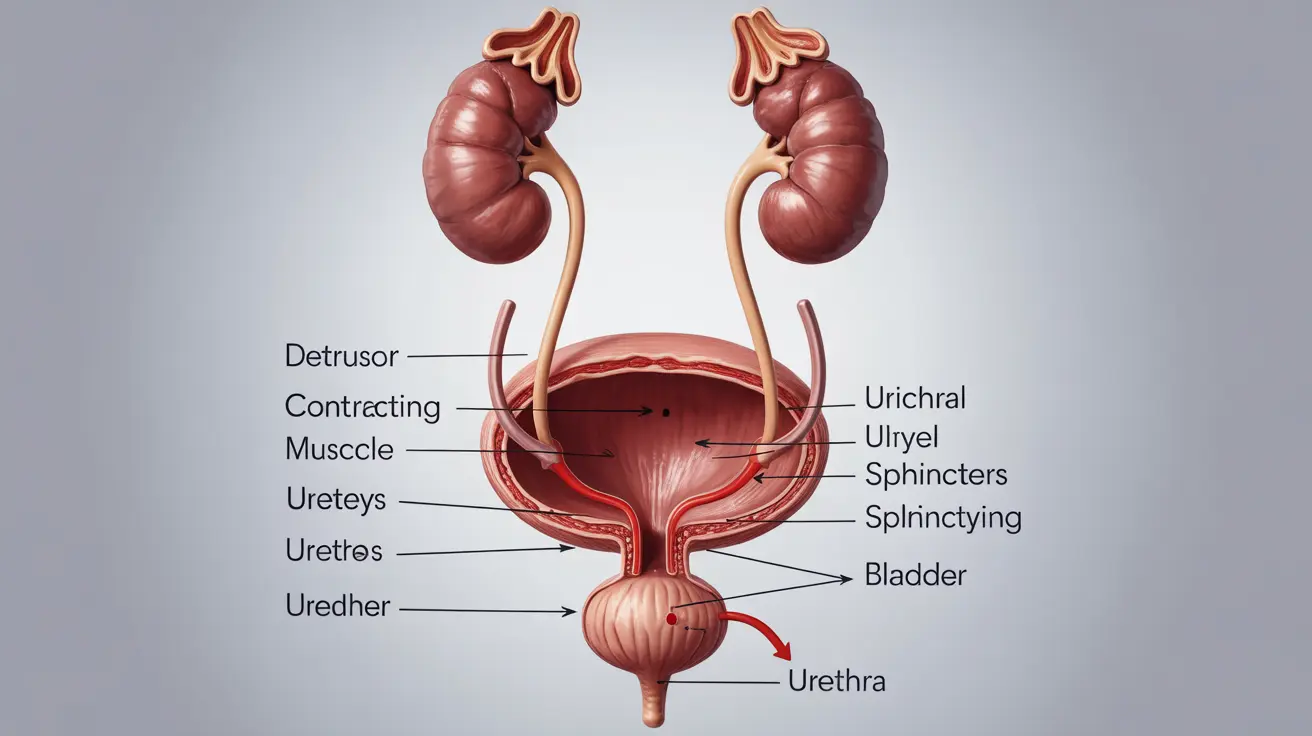
Normal urination begins when the bladder fills with urine produced by the kidneys. As the bladder expands, specialized receptors in the bladder wall send signals to the brain indicating the need to urinate. The brain then coordinates the complex process of voiding through the nervous system.
During healthy voiding, the detrusor muscle in the bladder wall contracts while the urethral sphincters simultaneously relax. This coordinated action allows urine to flow freely from the bladder through the urethra and out of the body. The entire process typically takes 20-40 seconds and should result in complete bladder emptying.
Several factors influence normal voiding patterns, including age, fluid intake, medications, and overall health status. Most adults urinate 6-8 times per day, with the ability to hold approximately 300-500 milliliters of urine comfortably before feeling the urge to void.
Recognizing Voiding Dysfunction Symptoms
Voiding dysfunction occurs when the normal urination process becomes impaired, leading to various uncomfortable and potentially serious symptoms. Common signs include difficulty initiating urination, weak or interrupted urine streams, and the sensation of incomplete bladder emptying after voiding.
Physical symptoms of voiding problems may include straining to urinate, prolonged urination time, or experiencing pain or burning during the process. Some people notice their urine stream starts and stops repeatedly or feels significantly weaker than normal.
Urinary retention, a severe form of voiding dysfunction, can cause additional symptoms such as lower abdominal pain, bloating, and the frequent urge to urinate with little actual urine output. In extreme cases, complete inability to void urine requires immediate medical attention.
Understanding Double Voiding Technique
Double voiding is a technique that can help people with incomplete bladder emptying improve their urination efficiency. This method involves urinating normally, waiting a few moments, then attempting to urinate again to empty any remaining urine from the bladder.
The double voiding technique works by allowing the bladder muscles to reset and contract again after the initial voiding attempt. During the brief waiting period, any remaining urine in the bladder can settle and become easier to expel during the second voiding attempt.
Healthcare providers often recommend double voiding for patients with conditions that affect bladder emptying, such as enlarged prostate, bladder weakness, or certain neurological conditions. While this technique can be helpful, it's important to consult with a medical professional to determine if it's appropriate for your specific situation.
Common Causes and Risk Factors
Multiple factors can contribute to difficulty voiding urine, ranging from temporary conditions to chronic medical problems. In men, prostate enlargement is one of the most common causes, as the enlarged gland can compress the urethra and obstruct urine flow.
Neurological conditions such as multiple sclerosis, spinal cord injuries, or stroke can disrupt the nerve signals that control bladder function. Medications including certain antihistamines, decongestants, and antidepressants may also interfere with normal voiding by affecting bladder muscle function or nerve signaling.
Women may experience voiding difficulties due to pelvic organ prolapse, urethral strictures, or complications following childbirth or surgery. Age-related changes in bladder function, chronic constipation, and urinary tract infections can affect people of any gender.
Diagnosis and Treatment Approaches
Diagnosing voiding dysfunction typically begins with a comprehensive medical history and physical examination. Healthcare providers may ask about urination patterns, fluid intake, medications, and any associated symptoms to better understand the underlying problem.
Diagnostic tests commonly include urinalysis, post-void residual measurement using ultrasound, and uroflowmetry to assess urine flow rate and pattern. More complex cases may require urodynamic studies, cystoscopy, or imaging studies to evaluate bladder and urethral function thoroughly.
Treatment options vary depending on the underlying cause and severity of symptoms. Conservative approaches may include pelvic floor exercises, bladder training techniques, dietary modifications, and medication adjustments. More severe cases might require medications to improve bladder function, medical devices, or surgical interventions.
Lifestyle modifications such as timed voiding schedules, proper hydration, and avoiding bladder irritants like caffeine and alcohol can significantly improve symptoms for many people. Working closely with healthcare providers ensures the most appropriate treatment plan for individual needs and circumstances.
Frequently Asked Questions
What does it mean to void urine and how does the normal urination process work?
To void urine means to empty the bladder by releasing urine from the body through urination. The normal process involves the bladder filling with urine, sending signals to the brain when full, and then coordinating the contraction of bladder muscles with the relaxation of urethral sphincters to allow urine to flow out completely.
What are the symptoms of voiding dysfunction and urinary retention?
Common symptoms include difficulty starting urination, weak or interrupted urine stream, straining to urinate, feeling of incomplete bladder emptying, frequent urination with small amounts, lower abdominal pain, and in severe cases, complete inability to urinate. Urinary retention may also cause bloating and significant discomfort.
What is double voiding and does it help with incomplete bladder emptying?
Double voiding is a technique where you urinate normally, wait a few moments, then attempt to urinate again to empty any remaining urine. This method can help people with incomplete bladder emptying by allowing bladder muscles to reset and contract again, potentially improving overall bladder emptying efficiency.
What causes difficulty voiding urine and who is at higher risk?
Common causes include prostate enlargement in men, neurological conditions, certain medications, pelvic organ prolapse in women, urethral strictures, and bladder muscle weakness. Higher risk factors include older age, neurological disorders, certain medications, history of pelvic surgery, chronic constipation, and conditions affecting the prostate or pelvic organs.
How is voiding dysfunction diagnosed and what are the treatment options?
Diagnosis typically involves medical history, physical examination, urinalysis, post-void residual measurement, and uroflowmetry. Treatment options range from conservative approaches like pelvic floor exercises and bladder training to medications that improve bladder function, medical devices, and surgical interventions depending on the underlying cause and severity of symptoms.