Kidney failure affects millions of Americans each year, representing one of the most serious health conditions that can develop gradually or strike suddenly. Understanding what causes kidney failure is crucial for early detection, prevention, and effective management of this life-threatening condition.
Your kidneys perform essential functions including filtering waste from your blood, regulating fluid balance, and producing hormones that control blood pressure. When kidney failure occurs, these vital organs lose their ability to function properly, leading to a dangerous buildup of toxins and fluid in your body.
Primary Causes of Kidney Failure
Diabetes: The Leading Culprit
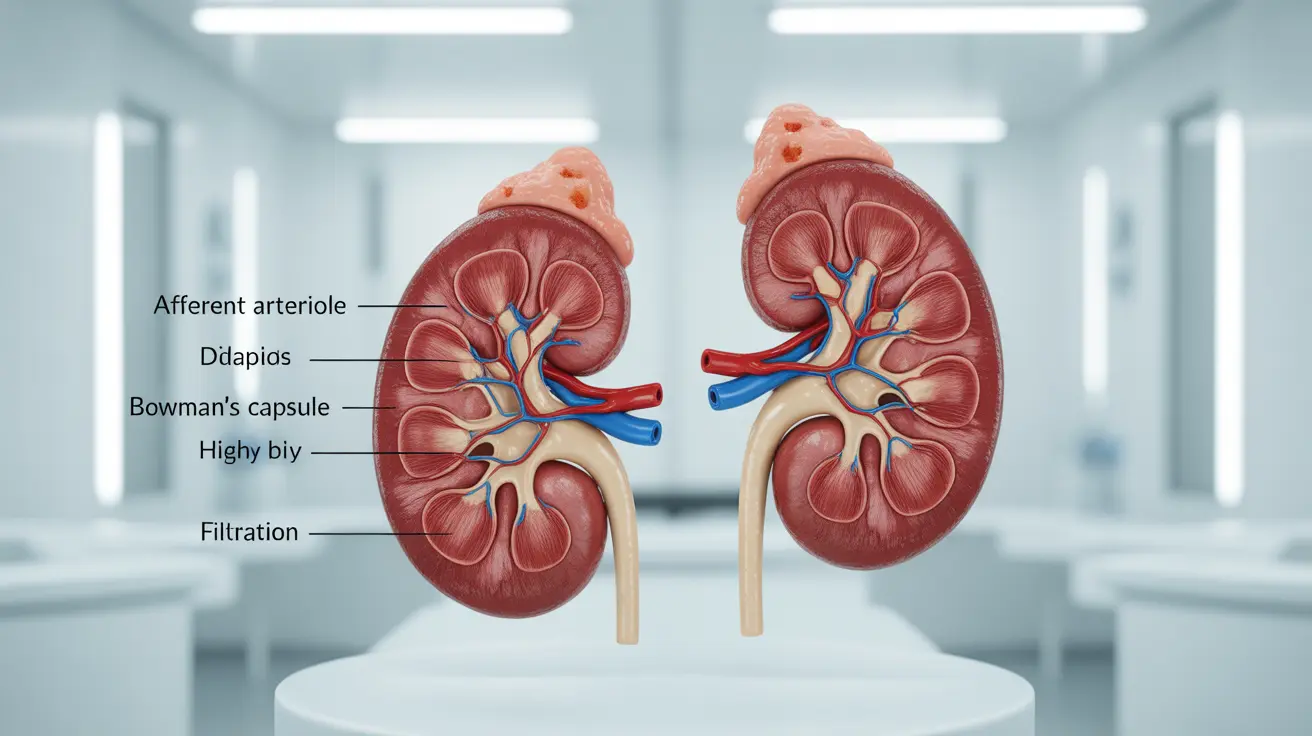
Diabetes stands as the number one cause of kidney failure in the United States, accounting for approximately 44% of all new cases. When blood sugar levels remain consistently elevated, they damage the tiny blood vessels in your kidneys called glomeruli. This damage occurs gradually over many years, often without noticeable symptoms in the early stages.
High glucose levels cause the kidney's filtering units to work harder than normal, leading to scarring and reduced function over time. This condition, known as diabetic nephropathy, typically develops 15-25 years after diabetes diagnosis, though it can occur sooner with poor blood sugar control.
High Blood Pressure: The Silent Destroyer
Hypertension ranks as the second leading cause of kidney failure, responsible for about 28% of cases. Your kidneys and blood pressure work together in a delicate balance - healthy kidneys help regulate blood pressure, while controlled blood pressure protects kidney function.
When blood pressure remains elevated, it damages the blood vessels throughout your kidneys, reducing their ability to filter blood effectively. This creates a dangerous cycle where kidney damage leads to higher blood pressure, which further damages the kidneys.
Understanding Acute Kidney Failure
Sudden Onset and Emergency Situations
Unlike chronic kidney disease that develops slowly over years, acute kidney failure can occur within hours or days. This medical emergency happens when your kidneys suddenly lose their filtering ability, causing waste products and fluid to accumulate rapidly in your body.
Common triggers for acute kidney failure include severe dehydration, blood loss, major surgery, certain medications (especially NSAIDs and some antibiotics), infections, and kidney stones that block urine flow. Hospital patients are particularly vulnerable, with acute kidney injury occurring in up to 20% of hospitalized individuals.
Medication-Related Kidney Damage
Several medications can cause acute kidney damage, especially when used long-term or in high doses. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen reduce blood flow to the kidneys, while certain antibiotics, chemotherapy drugs, and contrast dyes used in medical imaging can be directly toxic to kidney cells.
Recognizing Early Warning Signs
Physical Symptoms to Monitor
Early kidney failure often presents subtle symptoms that many people attribute to other causes. Fatigue and weakness occur as toxins build up in your bloodstream, while changes in urination patterns - including increased frequency, decreased output, or foamy urine - signal filtering problems.
Swelling in your ankles, feet, or around your eyes indicates fluid retention, while persistent nausea, loss of appetite, and metallic taste in your mouth reflect the accumulation of waste products your kidneys should be removing.
Laboratory Changes Before Symptoms
Blood tests often reveal kidney problems before symptoms appear. Rising levels of creatinine and blood urea nitrogen (BUN), along with decreased estimated glomerular filtration rate (eGFR), indicate declining kidney function. Protein in the urine (proteinuria) serves as an early warning sign of kidney damage.
Additional Risk Factors and Medical Conditions
Genetic and Hereditary Factors
Family history plays a significant role in kidney disease risk. Polycystic kidney disease, an inherited condition causing cysts to form in the kidneys, affects over 600,000 Americans. Other genetic conditions like Alport syndrome and certain forms of glomerulonephritis can also lead to kidney failure.
Autoimmune and Inflammatory Diseases
Lupus, an autoimmune disease, can cause lupus nephritis, leading to kidney inflammation and damage. Similarly, vasculitis (inflammation of blood vessels) can affect kidney blood vessels, while certain types of glomerulonephritis cause the kidney's filtering units to become inflamed.
Lifestyle and Environmental Factors
Chronic use of pain medications, exposure to heavy metals like lead or mercury, and certain herbal supplements can damage kidneys over time. Smoking accelerates kidney disease progression, while obesity increases the risk of developing diabetes and high blood pressure - both major kidney disease causes.
Prevention and Management Strategies
Controlling Diabetes and Blood Pressure
For people with diabetes, maintaining blood sugar levels within target ranges (typically HbA1c below 7%) significantly reduces kidney disease risk. This involves consistent medication adherence, regular blood sugar monitoring, and following a diabetes-friendly diet plan.
Blood pressure control requires maintaining readings below 130/80 mmHg for most adults, and even lower for those with existing kidney disease. ACE inhibitors and ARBs (angiotensin receptor blockers) provide additional kidney protection beyond blood pressure reduction.
Lifestyle Modifications for Kidney Health
A kidney-friendly diet emphasizes limiting sodium, phosphorus, and potassium while ensuring adequate protein intake. Regular physical activity helps control blood pressure and blood sugar while maintaining healthy weight. Staying well-hydrated supports kidney function, though fluid restrictions may be necessary in advanced kidney disease.
Avoiding nephrotoxic substances, including excessive NSAIDs, certain herbal supplements, and unnecessary contrast dyes, protects kidney function. Regular medical check-ups allow for early detection and intervention when kidney problems develop.
Frequently Asked Questions
What are the main causes of kidney failure and how do diabetes and high blood pressure contribute to it?
Diabetes and high blood pressure are the two leading causes of kidney failure. Diabetes damages kidney blood vessels through prolonged high blood sugar levels, while high blood pressure damages these same vessels through excessive force. Together, they account for over 70% of kidney failure cases. Both conditions create a harmful cycle where kidney damage worsens the underlying disease, accelerating kidney function decline.
How can acute kidney failure develop suddenly, and what are the common causes of this rapid kidney injury?
Acute kidney failure develops within hours to days when kidneys suddenly lose filtering ability. Common causes include severe dehydration, significant blood loss, major infections, certain medications (especially NSAIDs and some antibiotics), kidney stones blocking urine flow, and complications from surgery or medical procedures. Unlike chronic kidney disease, acute kidney injury often occurs in hospital settings and may be reversible with prompt treatment.
What are the early symptoms of kidney failure that people should watch for?
Early kidney failure symptoms include persistent fatigue, changes in urination (frequency, amount, or appearance), swelling in ankles or around eyes, nausea, loss of appetite, and metallic taste in the mouth. Many people also experience difficulty concentrating, muscle cramps, and shortness of breath. However, kidney disease often progresses silently, making regular blood tests crucial for early detection.
How can lifestyle changes or treatment help prevent or slow the progression of kidney failure caused by diabetes or high blood pressure?
Preventing kidney failure involves strict blood sugar control (HbA1c below 7%) for diabetics and maintaining blood pressure below 130/80 mmHg. Key lifestyle changes include following a kidney-friendly diet low in sodium and processed foods, exercising regularly, maintaining healthy weight, avoiding smoking, and limiting alcohol. Medications like ACE inhibitors or ARBs provide additional kidney protection beyond blood pressure control.
What other medical conditions or factors increase the risk of developing kidney failure besides diabetes and high blood pressure?
Additional risk factors include autoimmune diseases like lupus, inherited conditions such as polycystic kidney disease, chronic use of NSAIDs or certain medications, repeated kidney infections, kidney stones, family history of kidney disease, obesity, smoking, and age over 60. Certain ethnic groups, including African Americans, Hispanics, and Native Americans, face higher genetic risk for kidney disease development.