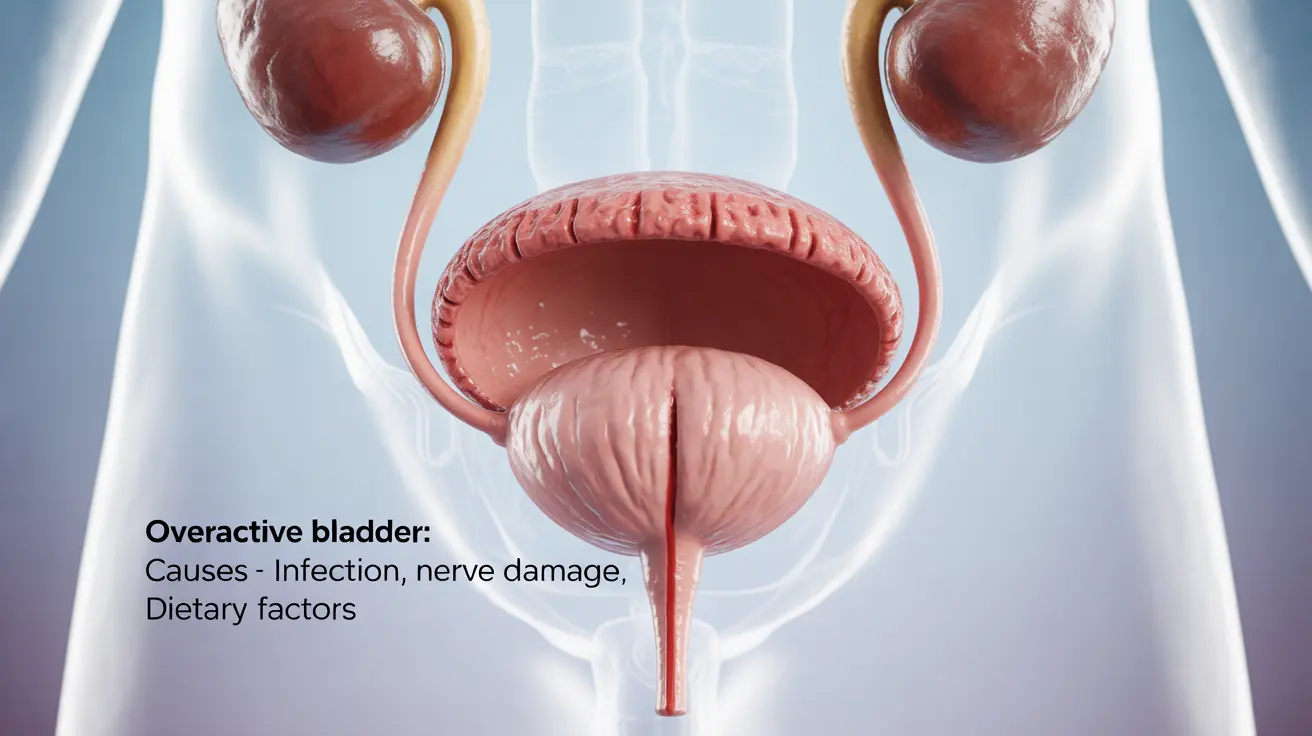
Overactive bladder (OAB) affects millions of Americans, significantly impacting their daily lives and routines. This common condition causes sudden urges to urinate that can be difficult to control, leading to anxiety and lifestyle limitations. Understanding what causes overactive bladder is crucial for proper diagnosis and effective treatment.
While many people experience OAB symptoms, the underlying causes can vary significantly from person to person. This comprehensive guide explores the various factors that contribute to overactive bladder and discusses available treatment options.
Common Causes of Overactive Bladder
Several factors can contribute to the development of overactive bladder symptoms:
Neurological Conditions
Neurological disorders often play a significant role in bladder control issues. Conditions such as multiple sclerosis, Parkinson's disease, stroke, and spinal cord injuries can disrupt the normal communication between the brain and bladder, leading to OAB symptoms.
Physical Conditions
Various physical conditions can trigger overactive bladder symptoms, including:
- Urinary tract infections (UTIs)
- Bladder obstruction
- Enlarged prostate in men
- Pelvic floor weakness
- Previous pelvic surgery
Age-Related Changes
As we age, the risk of developing overactive bladder increases. Changes in bladder muscle strength and overall nerve function can contribute to bladder control issues in older adults.
Diagnosis Process
Healthcare providers use various methods to diagnose overactive bladder and identify its underlying causes:
Medical History Review
Doctors begin by collecting detailed information about symptoms, medical history, and lifestyle factors that might contribute to bladder issues.
Physical Examination
A thorough physical exam may include:
- Neurological assessment
- Pelvic examination
- Prostate examination for men
- Assessment of pelvic floor strength
Diagnostic Tests
Several tests may be performed to confirm diagnosis and rule out other conditions:
- Urinalysis
- Bladder diary monitoring
- Urodynamic testing
- Post-void residual measurement
Treatment Approaches
Managing overactive bladder typically involves a combination of treatments:
Lifestyle Modifications
Initial treatment often focuses on behavioral changes:
- Scheduled bathroom visits
- Pelvic floor exercises
- Bladder training techniques
- Weight management if needed
Dietary Changes
Certain dietary modifications can help reduce symptoms:
- Limiting caffeine intake
- Reducing alcohol consumption
- Avoiding spicy foods
- Managing fluid intake timing
Medical Interventions
When lifestyle changes aren't sufficient, medical treatments may include:
- Anticholinergic medications
- Beta-3 agonists
- Botox injections
- Nerve stimulation therapy
Frequently Asked Questions
What are the most common causes of overactive bladder? The most common causes include neurological conditions, urinary tract infections, age-related changes, enlarged prostate in men, and pelvic floor weakness. Certain medications and lifestyle factors can also contribute to symptoms.
How is overactive bladder diagnosed by doctors? Doctors diagnose overactive bladder through a combination of medical history review, physical examination, urinalysis, bladder diary monitoring, and specialized urodynamic testing when necessary.
What are effective treatments and lifestyle changes for managing overactive bladder? Effective treatments include bladder training, pelvic floor exercises, dietary modifications, medications, and in some cases, more advanced therapies like Botox injections or nerve stimulation.
Can certain foods or drinks worsen symptoms of overactive bladder? Yes, several substances can aggravate symptoms, including caffeine, alcohol, artificial sweeteners, spicy foods, citrus fruits, and carbonated beverages. Managing fluid intake timing can also help control symptoms.
How do neurological conditions affect bladder control and lead to overactive bladder? Neurological conditions can disrupt the normal communication pathways between the brain and bladder, affecting proper muscle control and coordination. This disruption can lead to inappropriate bladder muscle contractions and OAB symptoms.