Hepatology is a specialized branch of medicine that focuses on the diagnosis, treatment, and management of diseases affecting the liver, gallbladder, biliary tree, and pancreas. This medical specialty has become increasingly important as liver disease rates continue to rise globally, making hepatologists essential healthcare providers in modern medicine.
Understanding what hepatology encompasses can help patients make informed decisions about their healthcare and recognize when specialized liver care might be necessary. Whether you're dealing with unexplained liver symptoms or have been referred to a hepatologist, this comprehensive guide will help you navigate this important medical field.
Understanding Hepatology and Its Focus Areas
Hepatology derives its name from the Greek word "hepato," meaning liver, combined with "logy," meaning study. While primarily focused on liver health, hepatologists also treat conditions affecting closely related organs that work together in the digestive system.
The liver serves as one of the body's most vital organs, performing over 500 essential functions including detoxification, protein synthesis, and bile production. When liver function becomes compromised, it can affect multiple body systems, making specialized care crucial.
Primary Organs in Hepatology Practice
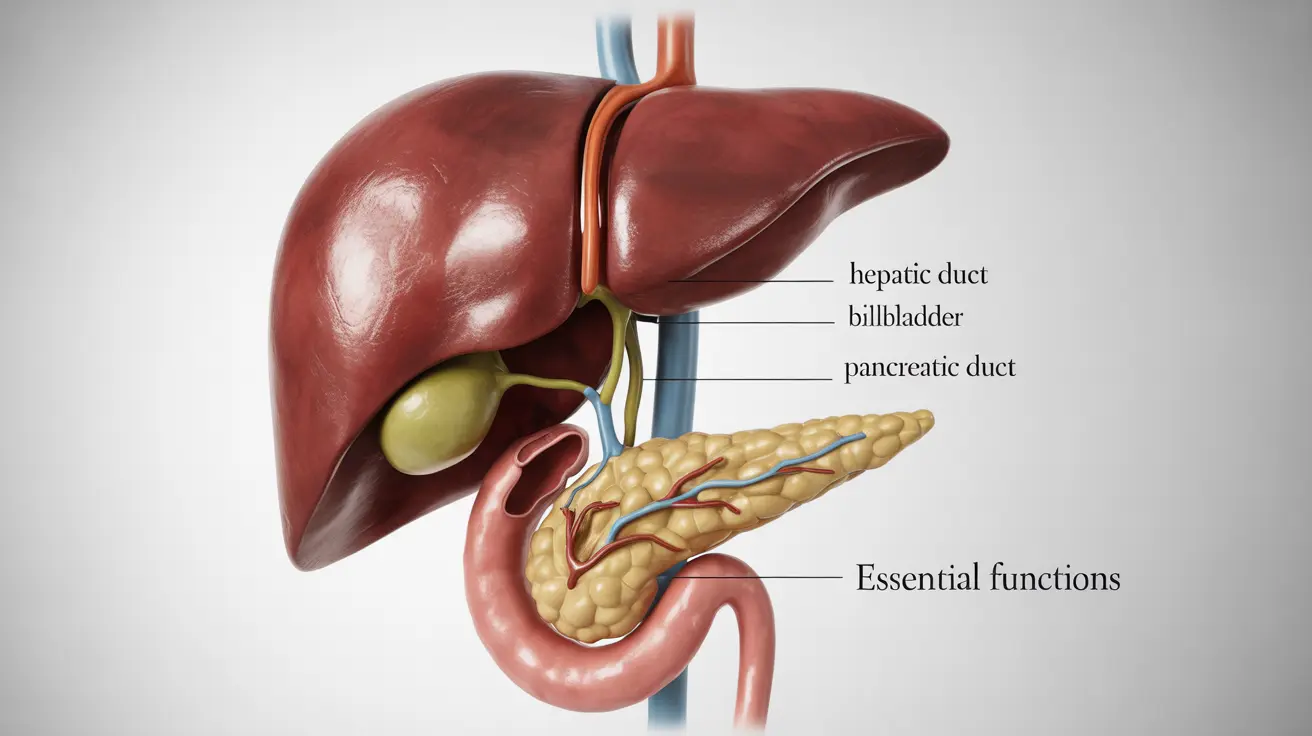
Hepatologists specialize in treating conditions affecting four main anatomical areas:
- The liver: The primary focus, including all liver tissue and blood vessels
- Gallbladder: The small organ that stores bile produced by the liver
- Biliary tree: The network of ducts that carry bile from the liver to the small intestine
- Pancreas: Particularly its role in digestion and bile duct connections
Common Conditions Treated by Hepatologists
Hepatologists manage a wide spectrum of liver and related diseases, ranging from acute infections to chronic progressive conditions. Their expertise covers both common and rare liver disorders that require specialized knowledge and treatment approaches.
Viral Hepatitis
Hepatitis viruses represent some of the most frequently treated conditions in hepatology. Hepatitis B and C infections can lead to chronic liver disease, cirrhosis, and liver cancer without proper management. Hepatologists provide antiviral treatments, monitor disease progression, and coordinate care to prevent complications.
Fatty Liver Disease
Non-alcoholic fatty liver disease (NAFLD) and alcoholic liver disease affect millions of Americans. These conditions involve fat accumulation in liver cells, potentially progressing to inflammation, scarring, and cirrhosis. Hepatologists develop comprehensive treatment plans addressing underlying causes and preventing disease advancement.
Cirrhosis and Advanced Liver Disease
When chronic liver conditions progress to cirrhosis, specialized hepatology care becomes critical. Hepatologists manage complications such as portal hypertension, ascites, and hepatic encephalopathy while evaluating patients for potential liver transplantation.
Autoimmune Liver Diseases
Conditions like autoimmune hepatitis, primary biliary cholangitis, and primary sclerosing cholangitis require immunosuppressive treatments and careful monitoring. Hepatologists have specialized training in managing these complex autoimmune conditions.
When to Seek Hepatologist Care
Recognizing when to consult a hepatologist can significantly impact treatment outcomes. While primary care physicians can manage basic liver concerns, certain situations warrant specialized hepatology expertise.
Elevated Liver Enzymes
Persistently elevated liver enzymes detected in blood tests often prompt referrals to hepatologists. These specialists can determine the underlying cause and develop appropriate treatment strategies when liver enzyme levels remain abnormally high despite initial interventions.
Chronic Liver Symptoms
Symptoms such as persistent fatigue, abdominal pain, jaundice, or unexplained weight loss may indicate liver disease requiring specialized evaluation. Hepatologists have advanced training in recognizing subtle signs of liver dysfunction that might be overlooked in general practice.
Complex Diagnostic Needs
When liver conditions require specialized diagnostic procedures such as liver biopsies, advanced imaging interpretation, or complex laboratory testing, hepatologists provide the necessary expertise and procedural skills.
Hepatology vs. Gastroenterology: Key Differences
While both specialties deal with digestive system disorders, important distinctions exist between hepatology and gastroenterology that affect patient care and treatment approaches.
Scope of Practice
Gastroenterologists treat disorders throughout the entire digestive tract, from the esophagus to the colon, while hepatologists focus specifically on liver, gallbladder, biliary, and pancreatic conditions. This specialized focus allows hepatologists to develop deeper expertise in liver disease management.
Training and Certification
Hepatologists complete additional fellowship training beyond gastroenterology residency, specializing exclusively in liver and related diseases. This extra training provides advanced skills in liver transplant evaluation, complex autoimmune liver diseases, and specialized therapeutic procedures.
Treatment Complexity
Hepatologists manage more complex liver conditions requiring specialized medications, advanced monitoring techniques, and coordination with liver transplant programs. Their focused expertise enables them to provide cutting-edge treatments not typically available in general gastroenterology practice.
Diagnostic Tests and Treatment Approaches
Modern hepatology employs sophisticated diagnostic tools and innovative treatment strategies to address liver diseases effectively. These advanced approaches enable precise diagnosis and personalized treatment plans.
Advanced Imaging Techniques
Hepatologists utilize specialized imaging studies including magnetic resonance elastography (MRE), which measures liver stiffness to assess fibrosis, and contrast-enhanced ultrasound for detailed liver lesion evaluation. These non-invasive techniques provide crucial diagnostic information while minimizing patient discomfort.
Laboratory Testing
Comprehensive hepatology evaluation includes specialized blood tests measuring liver function, viral markers, autoimmune antibodies, and genetic markers for inherited liver diseases. These tests help hepatologists identify specific disease patterns and monitor treatment responses.
Minimally Invasive Procedures
When tissue sampling is necessary, hepatologists perform liver biopsies using image-guided techniques that maximize diagnostic yield while minimizing complications. They also perform therapeutic procedures such as paracentesis for ascites management.
Innovative Treatments
Hepatology continues advancing with new antiviral medications for hepatitis C that achieve cure rates exceeding 95%, immunosuppressive protocols for autoimmune liver diseases, and emerging therapies for fatty liver disease. Hepatologists stay current with these rapidly evolving treatment options.
Frequently Asked Questions
What is hepatology and which organs does it focus on?
Hepatology is a medical specialty focused on diagnosing and treating diseases of the liver, gallbladder, biliary tree, and pancreas. While the liver is the primary organ of focus, hepatologists also manage conditions affecting the gallbladder, bile ducts, and pancreas due to their interconnected functions in digestion and metabolism.
What common liver diseases and conditions do hepatologists treat?
Hepatologists treat a wide range of conditions including viral hepatitis (B and C), fatty liver disease, cirrhosis, autoimmune liver diseases, liver cancer, genetic liver disorders, drug-induced liver injury, and complications of advanced liver disease such as portal hypertension and ascites.
When should I see a hepatologist instead of a general doctor or gastroenterologist?
You should consider seeing a hepatologist if you have persistently elevated liver enzymes, chronic liver disease, need liver transplant evaluation, have complex liver symptoms, require specialized liver procedures, or have been diagnosed with conditions like hepatitis B or C, autoimmune liver disease, or advanced cirrhosis.
How is hepatology different from gastroenterology?
While gastroenterology covers the entire digestive system, hepatology focuses specifically on liver, gallbladder, biliary, and pancreatic diseases. Hepatologists complete additional specialized fellowship training beyond gastroenterology and have deeper expertise in complex liver conditions, transplant evaluation, and advanced liver therapies.
What diagnostic tests and treatments are used by hepatologists for liver and related diseases?
Hepatologists use specialized imaging like MR elastography, comprehensive liver function tests, viral and autoimmune markers, liver biopsies, and advanced blood tests. Treatments include antiviral medications, immunosuppressive therapy, lifestyle interventions, management of cirrhosis complications, and coordination of liver transplant care when necessary.