When muscle weakness, twitching, or difficulty speaking develops, many people understandably fear they might have amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig's disease. However, numerous other medical conditions can produce symptoms that closely resemble those of ALS, leading to considerable anxiety and diagnostic challenges.
Understanding what mimics ALS is crucial for both patients and healthcare providers. While ALS is a serious progressive neurological condition, many of the disorders that share similar symptoms are treatable or even reversible when caught early. This knowledge can provide hope during the often lengthy diagnostic process and emphasize the importance of thorough medical evaluation.
Common Neurological Conditions That Mimic ALS
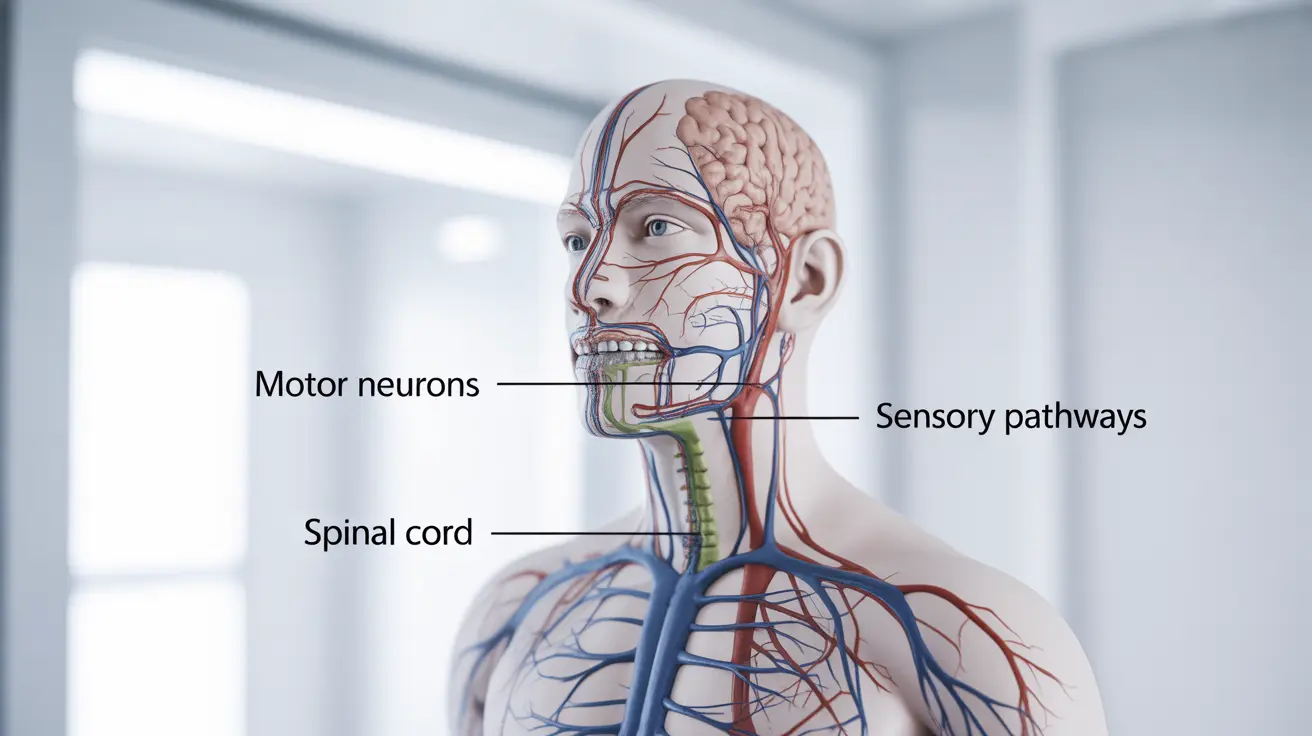
Several neurological disorders can present with muscle weakness, atrophy, or coordination problems similar to ALS. Multiple sclerosis (MS) frequently tops this list, as it can cause weakness, muscle spasms, and difficulty with movement. However, MS typically follows a relapsing-remitting pattern with periods of improvement, unlike the steadily progressive nature of ALS.
Myasthenia gravis represents another significant ALS mimic, causing muscle weakness that worsens with activity and improves with rest. This autoimmune condition particularly affects muscles controlling eye movement, facial expression, and swallowing. Unlike ALS, myasthenia gravis often responds dramatically to specific medications and treatments.
Spinal muscular atrophy (SMA) can also present similarly to ALS, especially in adult-onset forms. This genetic condition affects motor neurons but typically progresses more slowly than ALS and may have different patterns of muscle involvement.
Infectious and Inflammatory Causes
Lyme disease, caused by tick-borne bacteria, can produce neurological symptoms that mimic ALS, including muscle weakness and coordination problems. The key difference lies in Lyme disease's potential for complete recovery when treated appropriately with antibiotics, making early recognition vital.
Inflammatory conditions like polymyositis and inclusion body myositis can cause progressive muscle weakness similar to ALS. These conditions primarily affect muscle tissue rather than motor neurons and may respond to anti-inflammatory treatments or immunosuppressive therapy.
West Nile virus and other viral infections can occasionally cause ALS-like symptoms, particularly affecting motor neurons. While most viral-related symptoms resolve over time, some cases may leave lasting neurological effects.
Metabolic and Nutritional Deficiencies
Vitamin B12 deficiency stands out as one of the most important reversible causes of ALS-like symptoms. Severe B12 deficiency can damage the nervous system, causing weakness, numbness, and coordination problems. The encouraging news is that B12 replacement therapy can often reverse these symptoms if treatment begins before permanent nerve damage occurs.
Thyroid disorders, particularly hyperthyroidism, can cause muscle weakness, tremors, and fatigue that may initially resemble ALS symptoms. Thyroid function tests can quickly identify this treatable condition.
Magnesium deficiency can contribute to muscle twitching and weakness, while copper deficiency may cause neurological symptoms affecting movement and coordination. These nutritional imbalances are typically correctable with appropriate supplementation.
Structural and Mechanical Causes
Cervical spondylotic myelopathy occurs when age-related changes in the spine compress the spinal cord, potentially causing weakness and coordination problems in the arms and legs. Unlike ALS, this condition may improve with surgical intervention to relieve the compression.
Herniated discs or spinal stenosis can compress nerve roots, causing weakness and muscle atrophy in specific patterns. These mechanical problems often respond well to physical therapy, medications, or surgical procedures.
Brain tumors, particularly those affecting motor control areas, can occasionally present with progressive weakness resembling ALS. Advanced imaging studies can usually distinguish between these conditions.
Toxic Exposures and Medications
Certain medications can cause neurological side effects that mimic ALS symptoms. Statins, used for cholesterol management, rarely cause severe muscle problems. Some chemotherapy drugs can also affect nerve function, leading to weakness and coordination issues.
Heavy metal poisoning, including lead or mercury exposure, can cause neurological symptoms similar to ALS. Occupational or environmental exposure history often provides important clues for diagnosis.
Chronic alcohol use can lead to nutritional deficiencies and direct nerve damage, potentially causing weakness and muscle problems that resemble early ALS symptoms.
The Importance of Comprehensive Evaluation
Distinguishing between ALS and its mimics requires systematic medical evaluation. Healthcare providers typically begin with detailed medical history and physical examination, paying particular attention to symptom onset, progression patterns, and associated features.
The diagnostic process often involves multiple specialists, including neurologists, who can assess nerve and muscle function through specialized testing. Blood work can identify nutritional deficiencies, infections, or autoimmune conditions that might explain the symptoms.
Advanced imaging studies may reveal structural problems in the brain or spine, while electromyography (EMG) and nerve conduction studies can provide detailed information about nerve and muscle function.
Hope Through Accurate Diagnosis
While the diagnostic process for ALS-like symptoms can feel overwhelming, it's important to remember that many conditions causing these symptoms are treatable or reversible. Even when ALS is ultimately diagnosed, research continues to advance treatment options and improve quality of life for patients.
Working closely with healthcare providers throughout the evaluation process ensures the most accurate diagnosis and appropriate treatment plan. Early intervention for treatable conditions can make a significant difference in outcomes and long-term prognosis.
Frequently Asked Questions
What diseases and conditions can mimic the symptoms of ALS?
Multiple conditions can mimic ALS symptoms, including neurological disorders like multiple sclerosis, myasthenia gravis, and spinal muscular atrophy. Infectious diseases such as Lyme disease, nutritional deficiencies like vitamin B12 deficiency, thyroid disorders, spinal compression problems, and certain medications can also cause ALS-like symptoms. Each of these conditions has distinct characteristics that help differentiate them from true ALS.
How do doctors differentiate between ALS and disorders like myasthenia gravis or multiple sclerosis?
Doctors use several approaches to distinguish ALS from similar conditions. Clinical examination focuses on symptom patterns - myasthenia gravis typically worsens with activity and improves with rest, while multiple sclerosis often follows a relapsing-remitting course. Specialized tests like electromyography (EMG), nerve conduction studies, and specific blood tests for autoimmune markers help confirm diagnoses. MRI scans can reveal characteristic changes seen in multiple sclerosis but not typically in ALS.
What tests are used to rule out ALS when symptoms like muscle weakness and twitching appear?
The diagnostic workup typically includes comprehensive blood tests to check for vitamin deficiencies (especially B12), thyroid function, and autoimmune markers. Electromyography (EMG) and nerve conduction studies assess electrical activity in muscles and nerves. MRI scans of the brain and spinal cord can identify structural problems or signs of other neurological conditions. Additional tests may include spinal fluid analysis, genetic testing, or specialized antibody tests depending on suspected conditions.
Can conditions that mimic ALS be treated or reversed, and how does their prognosis compare?
Many ALS mimics have much better prognoses than ALS itself. Vitamin B12 deficiency can often be completely reversed with supplementation if caught early. Myasthenia gravis responds well to medications and treatments, with many patients achieving normal or near-normal function. Lyme disease can be cured with appropriate antibiotic treatment. Thyroid disorders are highly treatable with medication. Even structural problems like spinal compression may improve with surgery. This is why accurate diagnosis is so important - it can mean the difference between a progressive, incurable condition and a treatable one.
What are the key differences in symptoms between ALS and its common mimics such as vitamin B12 deficiency or Lyme disease?
ALS typically causes progressive weakness without sensory symptoms, starting in one area and spreading systematically. Vitamin B12 deficiency often includes numbness, tingling, and memory problems alongside weakness, and may affect sensation significantly. Lyme disease can cause fatigue, joint pain, and neurological symptoms that may fluctuate or improve partially over time. Unlike ALS, these conditions may have associated symptoms like rashes (Lyme), cognitive changes (B12 deficiency), or periods of improvement. The pattern and progression of symptoms often provide important clues for proper diagnosis.