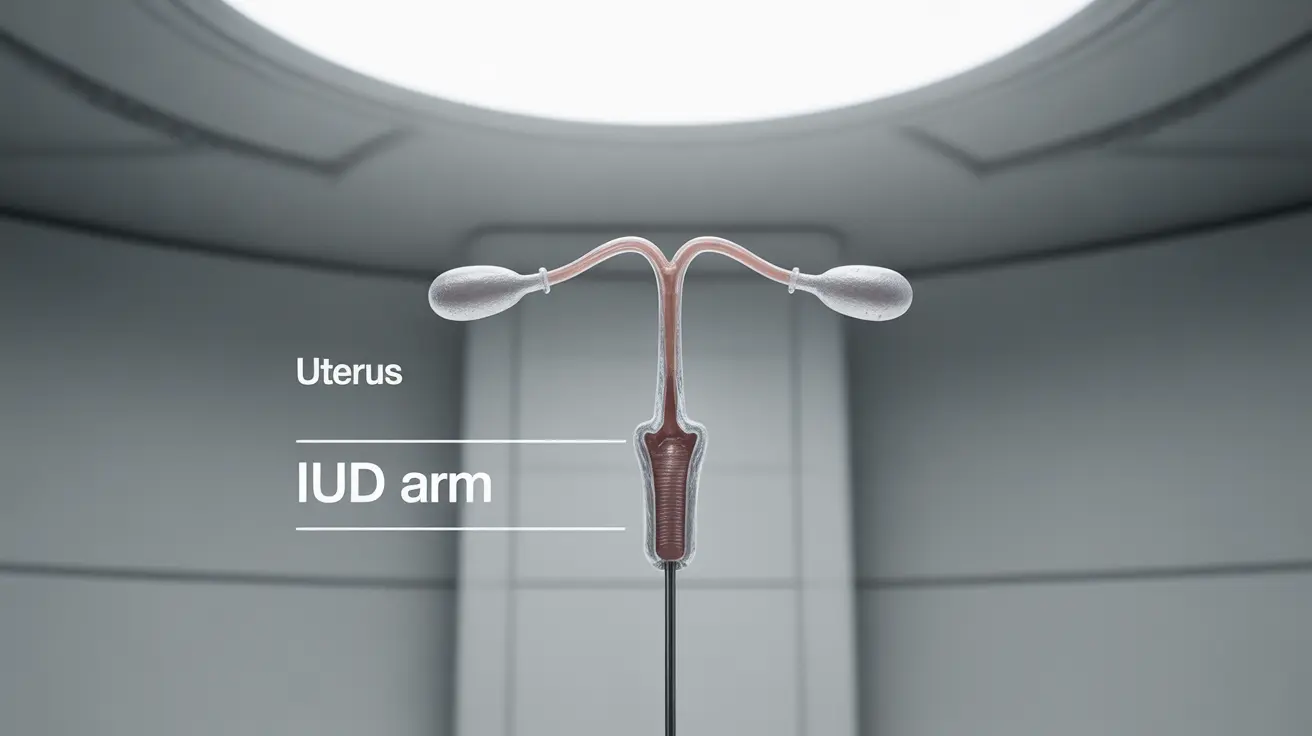
An intrauterine device (IUD) represents one of the most effective and low-maintenance forms of reversible birth control available today. This small, T-shaped device is placed in the uterus by a healthcare provider and can provide years of reliable contraception without requiring daily attention.
Whether you're considering an IUD for the first time or researching different birth control options, understanding how IUDs work, their types, and their potential effects can help you make an informed decision about your reproductive health.
How IUDs Work
IUDs prevent pregnancy through different mechanisms depending on their type. These devices work locally within the uterus to create an environment that prevents fertilization and implantation of eggs.
Mechanism of Action
Both types of IUDs create changes in the uterine environment that make it difficult for sperm to reach and fertilize an egg. They also alter the uterine lining in ways that prevent a fertilized egg from implanting.
Types of IUDs Available
Copper IUDs
The copper IUD is hormone-free and works by releasing small amounts of copper into the uterus. This creates an environment that's toxic to sperm while also preventing egg implantation. It's effective immediately after insertion and can remain in place for up to 10-12 years.
Hormonal IUDs
Hormonal IUDs release small amounts of progestin, which thickens cervical mucus, prevents ovulation in some cases, and thins the uterine lining. These IUDs come in different sizes and hormone levels, lasting between 3-7 years depending on the specific type.
IUD Effectiveness and Duration
IUDs are among the most effective forms of birth control, with success rates of over 99%. Once inserted, they begin working immediately and continue providing protection for several years, depending on the type:
- Copper IUDs: 10-12 years
- Hormonal IUDs: 3-7 years (varies by brand)
Common Side Effects and What to Expect
While IUDs are generally safe, some users may experience side effects, particularly in the first few months after insertion:
Initial Side Effects
- Cramping
- Irregular bleeding
- Spotting
- Heavier periods (with copper IUDs)
- Lighter or absent periods (with hormonal IUDs)
Long-term Considerations
Most side effects diminish within 3-6 months as your body adjusts to the device. Hormonal IUD users often experience lighter periods over time, while copper IUD users may have heavier periods initially.
Candidacy for IUD Use
IUDs are suitable for many women, including those who:
- Want long-term, reliable birth control
- Haven't had children
- Are breastfeeding
- Need emergency contraception (copper IUD only)
Frequently Asked Questions
What is an IUD and how does it work to prevent pregnancy?
An IUD is a small, T-shaped device inserted into the uterus that prevents pregnancy by either releasing copper (which is toxic to sperm) or hormones (which prevent ovulation and thicken cervical mucus). Both types create an environment that prevents fertilization and implantation.
What are the differences between copper and hormonal IUDs?
Copper IUDs use copper to prevent pregnancy, last 10-12 years, and contain no hormones. Hormonal IUDs release progestin, last 3-7 years, and often result in lighter periods. Copper IUDs may cause heavier periods, while hormonal IUDs typically reduce menstrual flow.
How long can IUDs remain effective and when should they be replaced?
Copper IUDs remain effective for 10-12 years, while hormonal IUDs last 3-7 years depending on the brand. They should be replaced at the end of their effective lifespan or removed earlier if pregnancy is desired.
What are common side effects of getting an IUD and how long do they last?
Common initial side effects include cramping, irregular bleeding, and spotting. These typically resolve within 3-6 months. Copper IUD users may experience heavier periods, while hormonal IUD users often have lighter or absent periods.
Who is a good candidate for an IUD and are there any people who should avoid using one?
IUDs are suitable for most women seeking long-term contraception, including those who haven't had children. However, they may not be appropriate for women with certain uterine abnormalities, active pelvic infections, or specific types of gynecological cancers.