Whipple disease is a rare but serious bacterial infection that primarily affects the small intestine, though it can impact multiple systems throughout the body. This complex condition, caused by the bacterium Tropheryma whipplei, requires prompt diagnosis and treatment to prevent potentially severe complications.
While this condition can affect anyone, it's most commonly diagnosed in middle-aged men and can be challenging to identify due to its diverse range of symptoms. Understanding its signs, diagnosis methods, and treatment options is crucial for both healthcare providers and patients.
What is Whipple Disease?
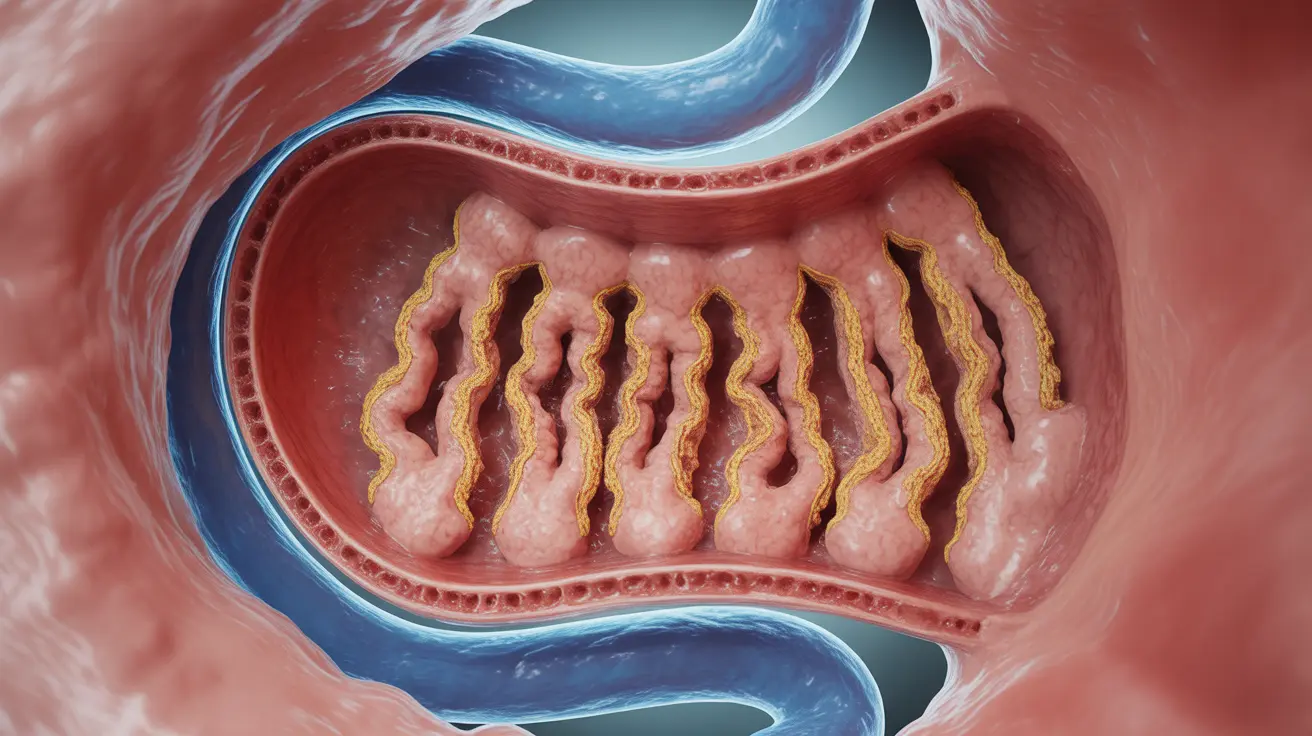
Whipple disease occurs when Tropheryma whipplei bacteria infect the body's tissues. The infection typically begins in the small intestine but can spread to various other organs and systems, including the heart, brain, joints, and eyes. The condition disrupts the body's ability to properly absorb nutrients, leading to malnutrition and various systemic problems.
Key Signs and Symptoms
The symptoms of Whipple disease can be wide-ranging and often develop gradually over time. Common manifestations include:
- Chronic diarrhea
- Unexplained weight loss
- Joint pain and swelling
- Fatigue and weakness
- Abdominal pain
- Enlarged lymph nodes
In more advanced cases, the disease can also cause:
- Neurological symptoms
- Vision problems
- Heart valve irregularities
- Skin darkening
- Chronic cough
Diagnosis Process
Diagnosing Whipple disease requires a comprehensive approach, as its symptoms can mimic many other conditions. The diagnostic process typically involves:
Physical Examination and Medical History
Doctors begin with a thorough physical examination and detailed review of symptoms and medical history. The pattern and progression of symptoms provide crucial diagnostic clues.
Diagnostic Tests
Several specific tests are used to confirm the presence of Whipple disease:
- Small intestine biopsy
- Polymerase chain reaction (PCR) testing
- Blood tests
- Imaging studies
Treatment Approaches
Treatment for Whipple disease primarily involves long-term antibiotic therapy. The standard treatment protocol includes:
Initial Treatment Phase
Patients typically receive intravenous antibiotics for 2-4 weeks, followed by oral antibiotics for 1-2 years. This extended treatment period is necessary to prevent relapse and ensure complete elimination of the bacteria.
Monitoring and Follow-up
Regular monitoring is essential during treatment to:
- Track symptom improvement
- Assess treatment effectiveness
- Monitor for potential side effects
- Check for signs of relapse
Long-term Management
Managing Whipple disease extends beyond the initial treatment phase. Patients need ongoing care and attention to:
- Monitor nutritional status
- Address any lingering symptoms
- Prevent potential complications
- Watch for signs of recurrence
Frequently Asked Questions
What are the common symptoms and early signs of Whipple disease?
Early signs typically include joint pain, chronic diarrhea, weight loss, and fatigue. These symptoms may develop gradually and can be easily mistaken for other conditions.
How is Whipple disease diagnosed and what tests are used to confirm it?
Diagnosis primarily relies on small intestine biopsy and PCR testing to detect the presence of T. whipplei bacteria. Additional tests may include blood work and imaging studies to assess the extent of organ involvement.
What is the standard treatment for Whipple disease and how long does it last?
Standard treatment involves initial intravenous antibiotics followed by long-term oral antibiotics, typically lasting 1-2 years total. The specific antibiotic regimen may vary based on individual cases.
Can Whipple disease be cured completely, and what are the risks of relapse?
While Whipple disease can be effectively treated, there is a risk of relapse if treatment is inadequate or discontinued too early. Complete cure is possible with proper adherence to the full course of antibiotics.
How does Whipple disease affect the digestive system and nutrient absorption?
The disease primarily affects the small intestine, damaging the villi that are responsible for nutrient absorption. This damage leads to malabsorption of nutrients, resulting in weight loss and various nutritional deficiencies.