Breast sensitivity is one of the most common concerns affecting people with breasts, yet it remains a topic many feel uncomfortable discussing openly. Whether you're experiencing sudden tenderness, cyclical discomfort, or ongoing sensitivity, understanding the underlying causes can help you find appropriate relief and determine when medical attention might be necessary.
From hormonal fluctuations to lifestyle factors, breast sensitivity can stem from numerous sources. While often temporary and manageable, persistent or severe breast tenderness sometimes signals underlying health conditions that warrant professional evaluation. Learning to distinguish between normal sensitivity and concerning symptoms empowers you to make informed decisions about your breast health.
Understanding Normal Breast Sensitivity
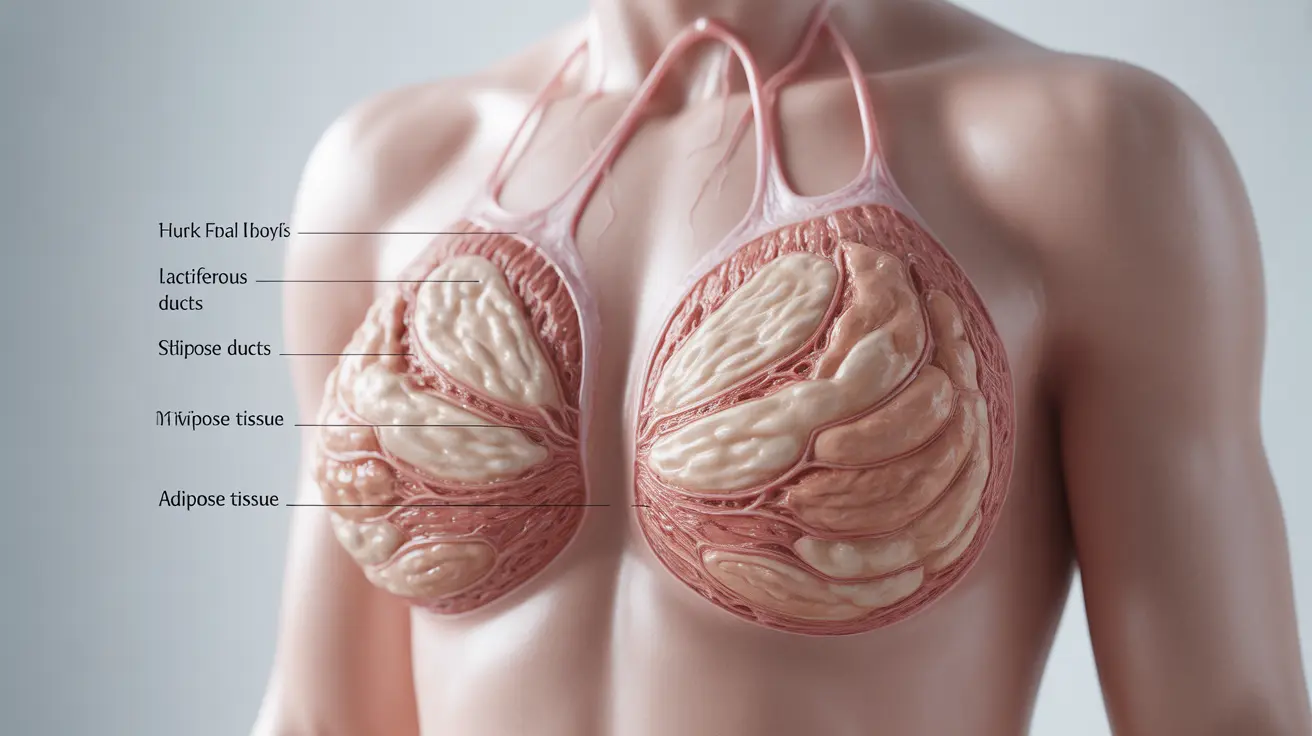
Breast tissue is naturally sensitive due to its complex structure of milk ducts, fatty tissue, and hormone receptors. This sensitivity can vary significantly throughout different life stages and hormonal cycles. Normal breast sensitivity typically presents as mild discomfort, slight swelling, or increased awareness of breast tissue without severe pain or concerning symptoms.
The degree of sensitivity often correlates with individual hormone levels, genetics, and breast tissue density. Some people naturally experience more sensitivity than others, and this baseline can change over time due to various factors including age, weight changes, and hormonal shifts.
Hormonal Causes of Breast Sensitivity
Menstrual Cycle Changes
The most common reason for breast sensitivity relates to natural hormonal fluctuations during the menstrual cycle. Estrogen and progesterone levels rise and fall throughout the month, directly affecting breast tissue. These hormones cause breast ducts to widen and breast tissue to swell, leading to tenderness that typically peaks in the days before menstruation.
This cyclical breast tenderness, medically known as mastalgia, affects up to 70% of menstruating individuals. The discomfort usually begins during the luteal phase of the cycle and resolves shortly after menstruation starts, when hormone levels drop.
Pregnancy and Breastfeeding
Pregnancy triggers dramatic hormonal changes that significantly impact breast sensitivity. Increased levels of human chorionic gonadotropin (hCG), estrogen, and progesterone cause rapid changes in breast tissue preparation for milk production. This sensitivity often appears as one of the earliest pregnancy symptoms.
During breastfeeding, breast sensitivity can result from engorgement, improper latch, blocked ducts, or hormonal adjustments. Postpartum hormone fluctuations, particularly the drop in estrogen and progesterone following delivery, can also contribute to ongoing breast tenderness.
Perimenopause and Menopause
The transition to menopause brings irregular hormone patterns that can intensify breast sensitivity. Fluctuating estrogen levels during perimenopause often cause more pronounced breast tenderness than experienced during regular menstrual cycles. After menopause, when estrogen levels stabilize at lower levels, breast sensitivity typically decreases significantly.
Medication-Related Breast Sensitivity
Various medications can trigger or worsen breast sensitivity by affecting hormone levels or directly impacting breast tissue. Birth control pills containing synthetic hormones often cause breast tenderness, particularly when starting a new formulation or adjusting dosages. This side effect usually diminishes after 2-3 months as the body adapts to the hormonal changes.
Hormone replacement therapy (HRT) commonly causes breast sensitivity due to the introduction of synthetic estrogen and progesterone. Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), can also contribute to breast tenderness by affecting prolactin levels and hormonal balance.
Other medications that may cause breast sensitivity include certain blood pressure medications, antipsychotic drugs, and fertility treatments. If you suspect medication is contributing to your breast tenderness, consult your healthcare provider about potential alternatives or dosage adjustments.
Lifestyle Factors and Breast Sensitivity
Diet, exercise habits, and stress levels can significantly influence breast sensitivity. Caffeine consumption has been linked to increased breast tenderness in some individuals, though scientific evidence remains mixed. High sodium intake can contribute to fluid retention, potentially worsening breast swelling and discomfort.
Physical activity levels also impact breast sensitivity. Inadequate breast support during exercise can cause trauma to breast tissue, leading to tenderness. Conversely, regular moderate exercise may help reduce overall breast tenderness by improving circulation and reducing stress hormones.
Stress management plays a crucial role in hormonal balance and breast sensitivity. Chronic stress elevates cortisol levels, which can interfere with normal hormone production and potentially worsen breast tenderness.
When to Seek Medical Attention
While breast sensitivity is often benign, certain symptoms warrant professional medical evaluation. Seek immediate medical attention if you experience sudden, severe breast pain accompanied by fever, redness, or warmth, as these may indicate infection.
Schedule a healthcare appointment if you notice persistent breast sensitivity lasting longer than one menstrual cycle, new lumps or changes in breast texture, nipple discharge (especially if bloody), or breast pain that interferes with daily activities. Additionally, any breast sensitivity accompanied by unexplained weight loss, persistent fatigue, or changes in breast size or shape should be evaluated promptly.
Breast sensitivity that occurs only on one side or in a specific area, rather than affecting both breasts generally, may also warrant medical investigation to rule out underlying conditions.
Effective Relief Strategies
Several evidence-based approaches can help manage breast sensitivity effectively. Proper bra fitting and support are fundamental, with studies showing that up to 85% of women wear incorrectly sized bras. A well-fitted, supportive bra can significantly reduce breast movement and associated discomfort.
Temperature therapy offers immediate relief for many people. Cold compresses can reduce swelling and numb pain, while warm compresses may improve circulation and relax tense breast tissue. Alternating between cold and warm applications often provides optimal comfort.
Over-the-counter pain relievers like ibuprofen or acetaminophen can effectively manage breast tenderness. Ibuprofen may be particularly beneficial due to its anti-inflammatory properties, which can address underlying tissue swelling contributing to sensitivity.
Dietary and Supplement Approaches
Certain dietary modifications may help reduce breast sensitivity. Limiting caffeine, reducing sodium intake, and maintaining adequate hydration can minimize fluid retention and associated breast swelling. Some studies suggest that evening primrose oil supplementation may help reduce cyclical breast pain, though results vary among individuals.
Vitamin E and vitamin B6 supplements have shown promise in some studies for reducing breast tenderness, particularly when related to premenstrual syndrome. However, consult with a healthcare provider before starting any supplement regimen to ensure safety and appropriate dosing.
Maintaining a balanced diet rich in fruits, vegetables, and whole grains while limiting processed foods and excessive sugar may help stabilize hormone levels and reduce overall inflammation that could contribute to breast sensitivity.
Frequently Asked Questions
Why are my boobs so sensitive before my period, and how can I get relief?
Breast sensitivity before your period occurs due to rising estrogen and progesterone levels that cause breast tissue to swell and become tender. For relief, try wearing a well-fitted supportive bra, applying cold or warm compresses, taking over-the-counter anti-inflammatory medication like ibuprofen, and reducing caffeine and salt intake. The sensitivity typically resolves once your period starts and hormone levels drop.
Can certain medications or birth control pills cause breast sensitivity or pain?
Yes, many medications can cause breast sensitivity, including hormonal birth control pills, hormone replacement therapy, antidepressants (especially SSRIs), certain blood pressure medications, and fertility treatments. Birth control pills are particularly common culprits due to synthetic hormones that can initially cause breast tenderness, though this often improves after 2-3 months of use.
What are the differences between normal breast sensitivity and signs I should see a doctor?
Normal breast sensitivity is typically mild to moderate, cyclical with your menstrual cycle, affects both breasts equally, and resolves on its own. See a doctor if you experience severe pain that interferes with daily activities, sensitivity lasting longer than one cycle, new lumps, nipple discharge, fever with breast pain, or sensitivity affecting only one breast or one specific area.
Are there home remedies or lifestyle changes that can help reduce breast tenderness?
Effective home remedies include wearing proper-fitting supportive bras, applying ice or heat therapy, gentle breast massage, taking warm baths, reducing caffeine and salt intake, staying hydrated, managing stress through relaxation techniques, and getting regular moderate exercise. Over-the-counter pain relievers and some supplements like evening primrose oil may also help.
Is it possible for breastfeeding, pregnancy, or hormonal changes to cause tender or sensitive breasts?
Absolutely. Pregnancy hormones like hCG, estrogen, and progesterone cause significant breast changes and sensitivity, often as an early pregnancy symptom. During breastfeeding, sensitivity can result from engorgement, blocked ducts, improper latch, or hormonal fluctuations. Perimenopause and menopause also commonly cause breast sensitivity due to irregular or changing hormone levels.