Menstrual cramps and period pain affect millions of women worldwide, ranging from mild discomfort to severe pain that can disrupt daily activities. Understanding why periods hurt and what causes this pain is crucial for managing symptoms effectively and knowing when to seek medical attention.
While period pain is a common experience, the underlying mechanisms and potential complications deserve careful attention. This comprehensive guide explores the causes of menstrual pain, warning signs to watch for, and evidence-based solutions for relief.
The Science Behind Period Pain
Period pain primarily occurs due to the natural processes happening in your uterus during menstruation. When your body releases an egg each month, the uterine lining builds up to prepare for potential pregnancy. If pregnancy doesn't occur, this lining needs to be shed, triggering a complex series of biological responses.
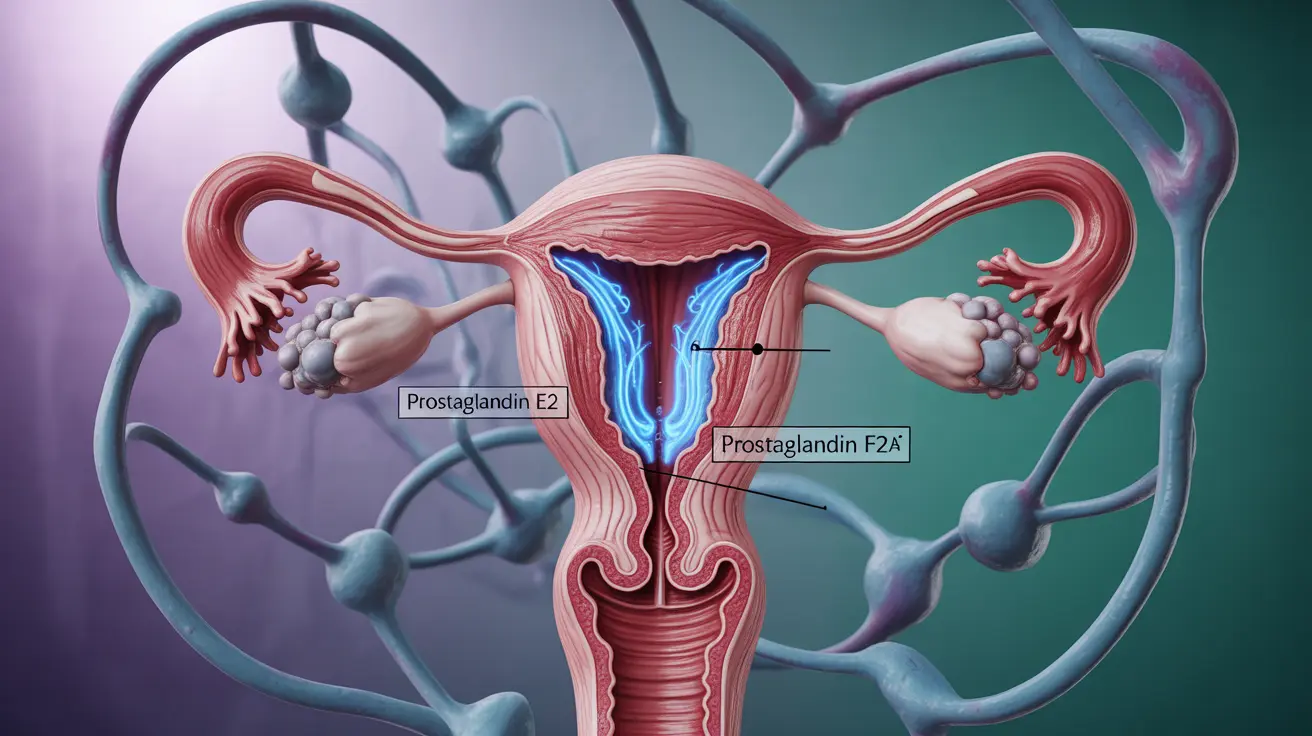
The Role of Prostaglandins
Prostaglandins are hormone-like substances that play a central role in period pain. These compounds cause the uterus to contract, helping to shed its lining. However, higher levels of prostaglandins can lead to stronger contractions and more intense pain. They can also cause other symptoms like nausea, diarrhea, and headaches.
Common Causes of Severe Period Pain
Primary Dysmenorrhea
Primary dysmenorrhea refers to typical menstrual cramps that aren't caused by other medical conditions. This type of pain usually begins a day or two before menstruation and can last for several days. The pain typically improves with age and after childbirth.
Secondary Dysmenorrhea
Secondary dysmenorrhea occurs when underlying medical conditions cause severe period pain. Common conditions include:
- Endometriosis
- Uterine fibroids
- Adenomyosis
- Pelvic inflammatory disease
- Cervical stenosis
Effective Treatment Options
Several treatment approaches can help manage period pain effectively:
Medication Options
- Over-the-counter pain relievers (NSAIDs)
- Hormonal birth control
- Prescription pain medication (in severe cases)
Natural Remedies and Lifestyle Changes
Many women find relief through natural methods and lifestyle modifications:
- Regular exercise
- Heat therapy (heating pads or warm baths)
- Dietary changes
- Stress reduction techniques
- Adequate sleep and rest
When to Seek Medical Help
While some period pain is normal, certain symptoms warrant medical attention:
- Severe pain that interferes with daily activities
- Pain lasting longer than usual
- Sudden changes in period pain intensity
- Heavy bleeding with clots
- Pain accompanied by fever or unusual discharge
Frequently Asked Questions
Why do periods hurt and what causes menstrual cramps?
Periods hurt primarily due to uterine contractions triggered by prostaglandins, which help shed the uterine lining. These contractions can temporarily reduce blood flow to the uterus, causing pain and cramping. The level of prostaglandins present determines the intensity of the pain.
What medical conditions can cause severe or persistent period pain?
Several medical conditions can cause severe period pain, including endometriosis, uterine fibroids, adenomyosis, and pelvic inflammatory disease. These conditions often require medical evaluation and specific treatment plans beyond standard pain management.
How do prostaglandins contribute to period pain and related symptoms?
Prostaglandins cause uterine muscle contractions and inflammation, leading to pain. They can also affect nearby organs, causing symptoms like nausea, diarrhea, and headaches. Higher levels of prostaglandins typically result in more severe symptoms.
When should I see a doctor about painful periods that do not improve?
Consult a healthcare provider if you experience severe pain that doesn't respond to over-the-counter medication, pain that interferes with daily activities, sudden changes in pain patterns, or if you develop new symptoms like heavy bleeding or fever.
What treatments or lifestyle changes can help reduce painful menstrual cramps?
Effective treatments include over-the-counter pain relievers, hormonal birth control, and lifestyle changes such as regular exercise, heat therapy, and stress management. Some women also find relief through dietary modifications and ensuring adequate rest during their period.