Wide pulse pressure is a cardiovascular measurement that many people don't fully understand, yet it can provide crucial insights into your heart health and overall well-being. This condition occurs when there's an unusually large difference between your systolic and diastolic blood pressure readings, typically defined as a gap of 60 mmHg or greater.
While blood pressure measurements are routine during medical visits, the pulse pressure component often receives less attention despite its significant implications for cardiovascular risk assessment. Understanding what wide pulse pressure means, its potential causes, and available management strategies can empower you to take proactive steps toward better heart health.
What Is Pulse Pressure and When Is It Considered Wide?
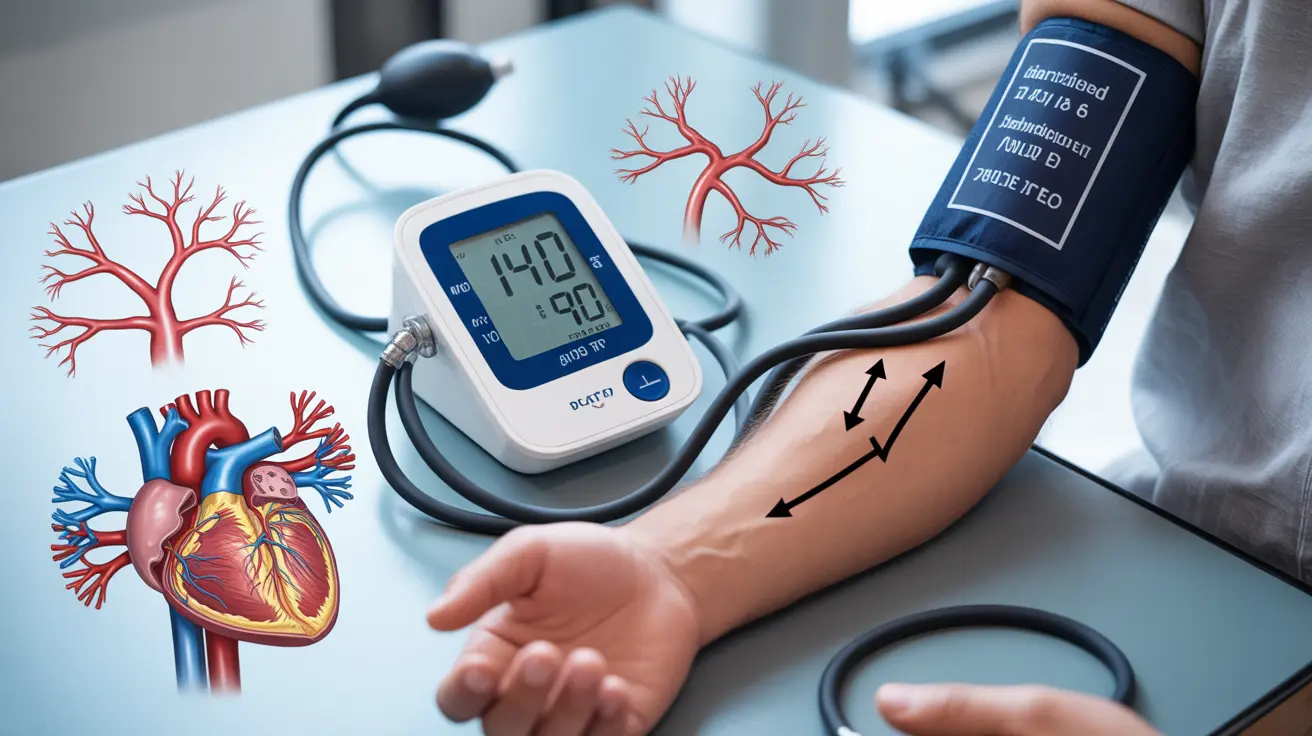
Pulse pressure represents the difference between your systolic blood pressure (the top number) and diastolic blood pressure (the bottom number). For example, if your blood pressure reading is 140/70 mmHg, your pulse pressure would be 70 mmHg. Medical professionals typically consider pulse pressure normal when it ranges between 30 to 50 mmHg.
A wide pulse pressure occurs when this difference exceeds 60 mmHg, though some healthcare providers may use slightly different thresholds based on individual patient factors. This measurement reflects the flexibility and function of your arteries, particularly the aorta, which is your body's largest artery.
The significance of pulse pressure lies in what it reveals about arterial stiffness and cardiovascular function. As we age, our arteries naturally become less elastic, but certain conditions can accelerate this process, leading to elevated pulse pressure readings that warrant medical attention.
Primary Causes Behind Wide Pulse Pressure
Several underlying conditions and factors can contribute to the development of wide pulse pressure. Understanding these causes is essential for proper diagnosis and treatment planning.
Age-Related Arterial Changes
The most common cause of wide pulse pressure is age-related arterial stiffening, also known as arteriosclerosis. As people age, the elastic fibers in arterial walls gradually deteriorate, making blood vessels less flexible and able to accommodate the heart's pumping action. This natural aging process typically becomes more pronounced after age 50.
Cardiovascular Conditions
Various heart and blood vessel conditions can lead to increased pulse pressure. Aortic valve regurgitation, where the heart's aortic valve doesn't close properly, allows blood to flow backward, creating a wider pressure differential. Hyperthyroidism can also increase pulse pressure by elevating heart rate and cardiac output while reducing peripheral resistance.
Lifestyle and Environmental Factors
Chronic high blood pressure, particularly isolated systolic hypertension, frequently results in wide pulse pressure. Additionally, factors such as excessive sodium intake, lack of physical activity, smoking, and chronic stress can contribute to arterial stiffening and elevated pulse pressure over time.
Recognizing Symptoms Associated With Wide Pulse Pressure
Many individuals with wide pulse pressure experience no obvious symptoms, which is why this condition is sometimes called a "silent" cardiovascular risk factor. However, some people may notice certain signs that could indicate elevated pulse pressure.
Common symptoms include persistent headaches, particularly in the morning, dizziness or lightheadedness when standing up quickly, and episodes of chest discomfort or palpitations. Some individuals report feeling unusually fatigued or experiencing shortness of breath during routine activities.
Visual disturbances, such as blurred vision or seeing spots, may occur in cases where wide pulse pressure is associated with significantly elevated systolic blood pressure. Nosebleeds, while less common, can also be a sign of severely elevated blood pressure readings.
It's important to note that these symptoms can be associated with many different health conditions, making regular blood pressure monitoring and professional medical evaluation crucial for accurate diagnosis and appropriate management.
Diagnostic Approaches and Accurate Measurement
Diagnosing wide pulse pressure requires accurate blood pressure measurement and comprehensive cardiovascular assessment. Healthcare providers use several approaches to evaluate this condition thoroughly.
Standard Blood Pressure Monitoring
The diagnosis typically begins with multiple blood pressure readings taken on different occasions using proper technique. Healthcare providers ensure patients are seated comfortably, with feet flat on the floor and the arm supported at heart level. Multiple readings help account for normal blood pressure variations throughout the day.
Advanced Diagnostic Testing
When wide pulse pressure is identified, additional tests may be necessary to determine underlying causes. These can include echocardiograms to assess heart valve function and cardiac structure, thyroid function tests to rule out hyperthyroidism, and arterial stiffness measurements using specialized equipment.
Some healthcare providers may recommend 24-hour ambulatory blood pressure monitoring to obtain a comprehensive picture of blood pressure patterns throughout daily activities and sleep cycles. This extended monitoring can reveal important information not captured during single office visits.
Treatment Options and Management Strategies
Managing wide pulse pressure typically involves addressing underlying causes while implementing strategies to improve arterial flexibility and overall cardiovascular health. Treatment approaches are often individualized based on specific patient factors and contributing conditions.
Medication Management
When wide pulse pressure is associated with high blood pressure, healthcare providers may prescribe antihypertensive medications. ACE inhibitors and calcium channel blockers are often preferred because they can help reduce arterial stiffness while lowering blood pressure. Beta-blockers may be used in specific situations, though they can sometimes increase pulse pressure.
For patients with underlying thyroid disorders, appropriate thyroid hormone regulation is essential. Those with aortic valve problems may require specialized cardiac medications or, in severe cases, surgical intervention.
Lifestyle Modifications
Dietary changes play a crucial role in managing wide pulse pressure. Reducing sodium intake to less than 2,300 mg per day, and ideally closer to 1,500 mg for those with hypertension, can help improve blood pressure control. Increasing potassium-rich foods, such as bananas, leafy greens, and beans, may also provide cardiovascular benefits.
Regular physical activity, particularly aerobic exercise, can help improve arterial flexibility and reduce pulse pressure over time. Healthcare providers typically recommend at least 150 minutes of moderate-intensity exercise per week, though individual exercise prescriptions may vary based on overall health status.
Stress management techniques, including meditation, deep breathing exercises, and adequate sleep, can contribute to better blood pressure control and cardiovascular health. Smoking cessation is absolutely essential, as tobacco use significantly accelerates arterial stiffening and increases cardiovascular risk.
Frequently Asked Questions
What does a wide pulse pressure mean for my heart health and risks?
Wide pulse pressure indicates increased arterial stiffness and can significantly elevate your risk of cardiovascular events, including heart attack, stroke, and heart failure. It suggests that your arteries are less flexible and may not be functioning optimally. This condition is associated with a 20-30% increased risk of major cardiovascular events compared to normal pulse pressure. However, with proper management and lifestyle changes, these risks can be substantially reduced.
What are the common causes of wide pulse pressure?
The most common causes include age-related arterial stiffening, isolated systolic hypertension, aortic valve regurgitation, and hyperthyroidism. Other contributing factors include chronic high blood pressure, diabetes, kidney disease, and lifestyle factors such as smoking, excessive alcohol consumption, and lack of physical activity. In some cases, certain medications or genetic factors may also contribute to elevated pulse pressure.
What symptoms might I notice if I have a wide pulse pressure?
Many people with wide pulse pressure experience no symptoms at all. When symptoms do occur, they may include morning headaches, dizziness upon standing, chest discomfort, palpitations, fatigue, shortness of breath during normal activities, and occasionally visual disturbances or nosebleeds. These symptoms are often subtle and can be easily attributed to other causes, which is why regular blood pressure monitoring is important.
How is wide pulse pressure diagnosed and measured accurately?
Wide pulse pressure is diagnosed through careful blood pressure measurement, typically requiring multiple readings on separate occasions. Healthcare providers use standardized techniques with properly calibrated equipment and ensure proper patient positioning. Additional tests may include echocardiograms, thyroid function tests, and arterial stiffness assessments. Some patients may benefit from 24-hour ambulatory blood pressure monitoring to capture comprehensive blood pressure patterns.
What treatments and lifestyle changes can help manage wide pulse pressure?
Treatment typically involves medications such as ACE inhibitors or calcium channel blockers to address high blood pressure and improve arterial flexibility. Lifestyle modifications are equally important and include reducing sodium intake, increasing physical activity, maintaining a healthy weight, managing stress, getting adequate sleep, and avoiding tobacco and excessive alcohol. Regular monitoring and working closely with healthcare providers to adjust treatment plans as needed is essential for optimal management.