Eye parasites, including various types of worms, represent a concerning but treatable medical condition that can affect people worldwide. While relatively uncommon in developed countries, parasitic infections of the eye occur more frequently in tropical and subtropical regions where certain species of worms thrive.
Understanding the signs, causes, and treatment options for a worm in eye infections is crucial for prompt medical intervention and successful recovery. These infections can range from mild irritation to serious complications if left untreated, making early recognition and proper medical care essential.
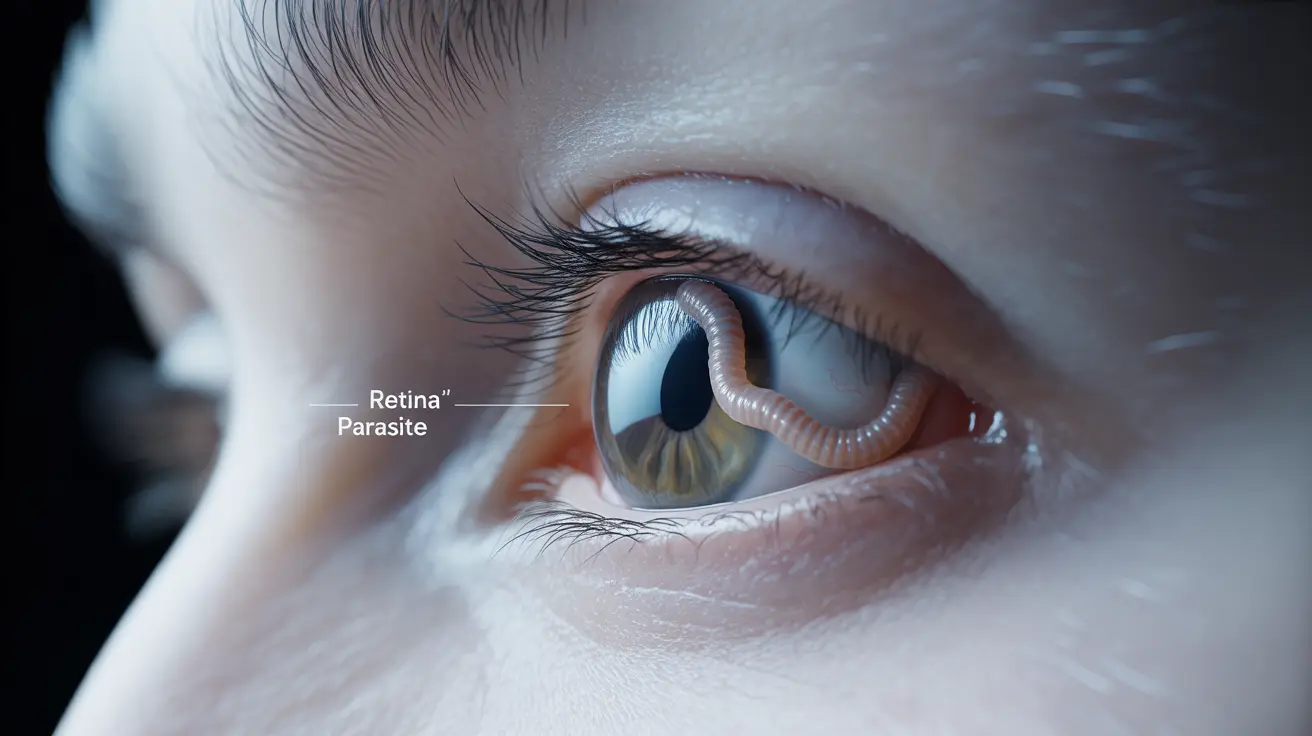
Understanding Eye Parasites and Worm Infections
Several types of parasitic worms can infect the human eye, with the most common being Loa loa (African eye worm), Onchocerca volvulus (river blindness), and Thelazia species. These parasites typically enter the body through insect bites, contaminated water, or poor hygiene practices, eventually migrating to the eye area.
The eye provides an ideal environment for certain parasites due to its warm, moist conditions and rich blood supply. When worms establish themselves in ocular tissues, they can cause inflammation, discomfort, and potentially severe vision problems if not addressed promptly by medical professionals.
Recognizing the Symptoms of Eye Worm Infections
Identifying a worm in eye infection requires awareness of both visible and symptomatic indicators. Early detection significantly improves treatment outcomes and prevents complications that could affect long-term vision health.
Visible Signs and Physical Symptoms
The most obvious sign of an eye worm infection is actually seeing the parasite moving across the surface of the eye or under the eyelid. This movement typically appears as a thin, thread-like organism that may be visible to the naked eye or detected during routine eye examinations.
Other common physical symptoms include persistent eye irritation, excessive tearing, redness, and swelling around the affected eye. Patients often experience a sensation of something moving in their eye, accompanied by itching or burning sensations that worsen over time.
Systemic and Secondary Symptoms
Beyond localized eye symptoms, patients may develop secondary signs including sensitivity to light, blurred vision, and difficulty focusing. Some individuals experience headaches, particularly around the affected eye area, and may notice changes in their peripheral vision.
In cases involving certain parasite species, patients might also develop skin nodules or experience generalized itching as the infection progresses. These systemic symptoms often indicate that the parasitic infection has spread beyond the initial eye area.
Common Causes and Risk Factors
Understanding how worms enter the eye helps individuals take appropriate preventive measures and recognize their risk level for developing these infections.
Insect-Transmitted Infections
Many eye worm infections result from bites by infected insects, particularly flies, mosquitoes, and blackflies that serve as intermediate hosts for various parasitic species. These insects pick up parasite larvae from infected animals or humans and transmit them during subsequent blood meals.
Geographic location plays a significant role in infection risk, with tropical and subtropical regions showing higher incidence rates due to favorable conditions for both parasites and their insect vectors. Travelers to these areas face increased exposure, especially during outdoor activities in rural or forested regions.
Contaminated Water and Poor Hygiene
Some eye worm infections occur through contact with contaminated water sources, particularly in areas with inadequate sanitation systems. Swimming or washing in infected water can introduce parasites directly to the eye area, while poor hand hygiene can facilitate transfer from contaminated surfaces.
Contact lens users face additional risks if they fail to maintain proper lens hygiene or use contaminated water for cleaning. Improper storage and cleaning of contact lenses can create environments where parasites survive and eventually reach the eye.
Treatment Approaches for Eye Worm Infections
Successful treatment of a worm in eye infection requires professional medical intervention, typically involving specialized medications and, in some cases, surgical procedures to remove the parasites completely.
Antiparasitic Medications
Medical professionals typically prescribe specific antiparasitic drugs based on the type of worm identified through laboratory testing. Common medications include ivermectin, albendazole, and diethylcarbamazine, each targeting different parasitic species with varying effectiveness.
Treatment duration and dosage depend on the severity of infection, patient health status, and specific parasite species involved. Patients must complete the full medication course even if symptoms improve, as incomplete treatment can lead to recurring infections or drug resistance.
Surgical Intervention Options
In cases where worms are visible and accessible, surgical removal may provide immediate relief and prevent further complications. This outpatient procedure typically involves local anesthesia and careful extraction of the parasite using specialized instruments.
More complex cases might require advanced surgical techniques, particularly when parasites have established themselves in deeper eye tissues. Post-surgical care includes antibiotic treatments to prevent secondary bacterial infections and regular follow-up appointments to monitor healing progress.
Prevention Strategies and Risk Reduction
Preventing eye worm infections focuses on avoiding exposure to parasites and their insect vectors while maintaining excellent hygiene practices, particularly when traveling to high-risk areas.
Travel Precautions and Environmental Awareness
Travelers to tropical regions should use comprehensive insect protection, including DEET-based repellents, long-sleeved clothing, and bed nets treated with insecticides. Avoiding outdoor activities during peak insect activity periods, typically dawn and dusk, significantly reduces exposure risk.
Staying in well-screened accommodations and avoiding areas near stagnant water sources helps minimize contact with disease-carrying insects. Travelers should also avoid swimming or bathing in potentially contaminated water sources, opting for chlorinated pools or properly treated water when available.
Personal Hygiene and Eye Care
Maintaining excellent hand hygiene prevents accidental transfer of parasites to the eye area, while proper contact lens care eliminates contamination risks. Users should follow manufacturer guidelines strictly and never use tap water for lens cleaning or storage.
Regular eye examinations help detect early signs of infection before symptoms become severe, particularly important for individuals living in or frequently traveling to high-risk regions. Prompt medical attention for any unusual eye symptoms can prevent complications and ensure appropriate treatment.
Frequently Asked Questions
What are the symptoms of a worm in the eye, and how do I know if I'm infected?
The most distinctive symptom is actually seeing a thin, thread-like worm moving across your eye or under your eyelid. Other symptoms include persistent eye irritation, excessive tearing, redness, swelling, light sensitivity, blurred vision, and the sensation of something moving in your eye. You might also experience itching, burning sensations, and headaches around the affected eye area.
Can you get a worm in your eye from eating undercooked food or poor contact lens hygiene?
While eating undercooked food can cause other types of parasitic infections, eye worms typically enter through insect bites from infected flies, mosquitoes, or blackflies. However, poor contact lens hygiene can increase your risk if you use contaminated water to clean lenses or store them improperly. The main transmission routes are insect bites and direct contact with contaminated water sources.
How is a worm in the eye treated, and what medicines or surgeries are available?
Treatment typically involves antiparasitic medications such as ivermectin, albendazole, or diethylcarbamazine, prescribed based on the specific parasite species identified. In cases where the worm is visible and accessible, doctors may surgically remove it using local anesthesia and specialized instruments. More complex cases might require advanced surgical procedures, followed by antibiotics to prevent secondary infections.
What steps can I take to prevent getting a worm in my eye, especially when traveling to tropical areas?
Use comprehensive insect protection including DEET-based repellents, wear long-sleeved clothing, and sleep under insecticide-treated bed nets. Avoid outdoor activities during dawn and dusk when insects are most active. Stay in well-screened accommodations, avoid swimming in potentially contaminated water sources, maintain excellent hand hygiene, and follow proper contact lens care guidelines if you wear them.
Is it possible to have a worm in your eye without noticing any symptoms, and when should I see a doctor?
While some early infections might cause minimal symptoms, most eye worm infections eventually produce noticeable signs like irritation, tearing, or visible movement. You should see a doctor immediately if you notice any unusual eye symptoms, especially after traveling to tropical regions, see something moving in your eye, experience persistent irritation or vision changes, or develop unexplained eye redness and swelling.