Experiencing breast pain after menopause can be concerning, especially since many women expect breast discomfort to diminish once their menstrual cycles end. While postmenopausal breast pain is relatively common, understanding its causes and knowing when to seek medical attention is crucial for maintaining breast health and peace of mind.
This comprehensive guide will explore the various aspects of postmenopausal breast pain, including its causes, management strategies, and important warning signs that warrant medical attention.
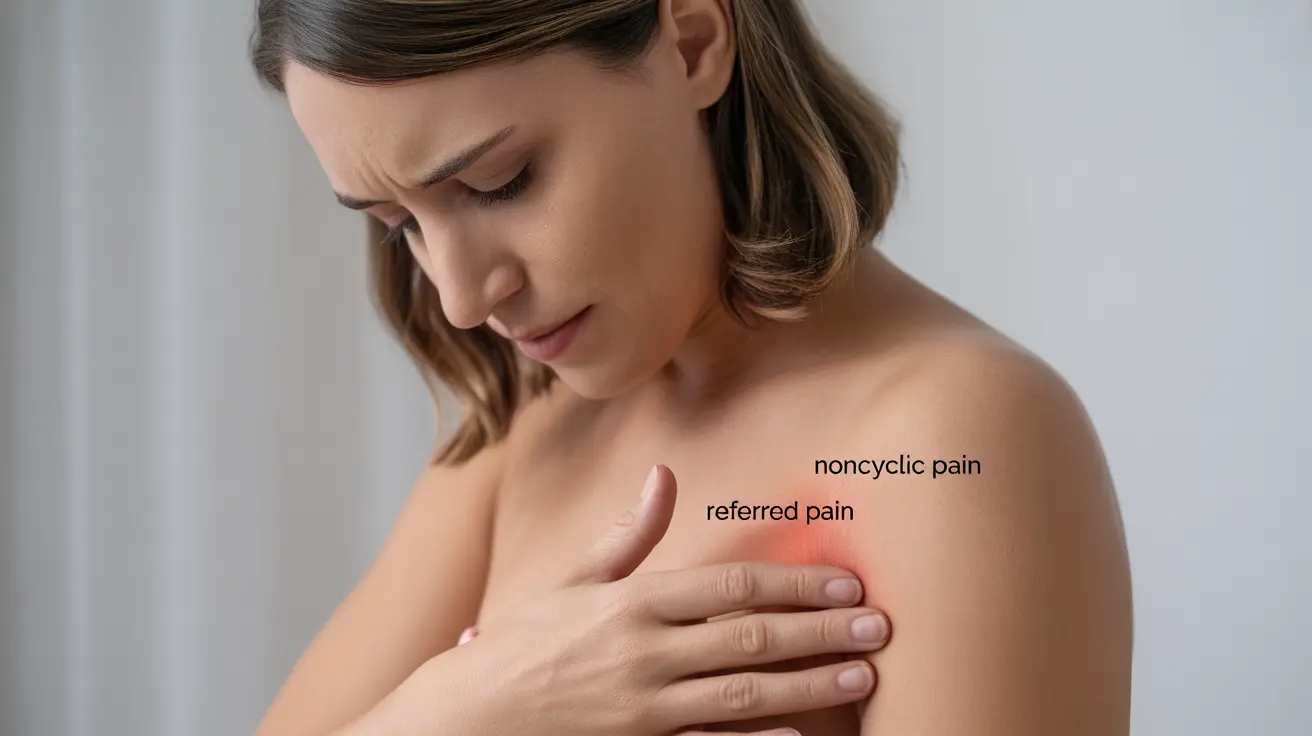
Types of Postmenopausal Breast Pain
Breast pain after menopause typically falls into two main categories: noncyclic and referred pain. Unlike premenopausal breast pain, which often follows hormonal cycles, postmenopausal breast pain tends to be more sporadic and may have different underlying causes.
Noncyclic Breast Pain
This type of pain is usually localized to a specific area of the breast and may be described as burning, sharp, or tender. It can be caused by various factors, including:
- Medications
- Injury or trauma
- Breast cysts
- Previous breast surgery
- Chest wall pain
Referred Pain
Sometimes, breast pain may actually originate from another area of the body, such as:
- Muscle strain
- Costochondritis (inflammation of chest wall cartilage)
- Spine problems
- Heart-related conditions
Common Causes of Postmenopausal Breast Pain
Several factors can contribute to breast pain after menopause:
Hormone-Related Causes
Even after menopause, hormonal fluctuations can still occur, especially in women taking:
- Hormone replacement therapy (HRT)
- Certain medications that affect hormone levels
- Natural supplements with phytoestrogens
Physical Causes
Many physical factors can lead to breast discomfort:
- Poor-fitting bras
- Weight changes
- Breast cysts or fibroadenomas
- Physical activity-related strain
Managing Postmenopausal Breast Pain
Several strategies can help alleviate breast pain after menopause:
Lifestyle Modifications
- Wearing properly fitted, supportive bras
- Maintaining a healthy weight
- Regular gentle exercise
- Limiting caffeine intake
- Using warm or cold compresses
Medical Interventions
When necessary, medical treatments may include:
- Adjusting hormone replacement therapy dosage
- Over-the-counter pain relievers
- Prescription medications
- Treatment of underlying conditions
Warning Signs and Red Flags
While most postmenopausal breast pain is benign, certain symptoms warrant immediate medical attention:
- New, persistent pain in one specific area
- Pain accompanied by lumps or skin changes
- Nipple discharge or changes
- Breast inflammation or redness
- Pain that interferes with daily activities
Frequently Asked Questions
- What are the common causes of breast pain after menopause, and how is it typically different from premenopausal breast pain?
Postmenopausal breast pain is usually noncyclic and may be caused by hormonal changes, medications, physical factors, or underlying medical conditions. Unlike premenopausal pain, it doesn't typically follow a monthly pattern and is more likely to be localized to specific areas.
- How can I manage or relieve breast pain after menopause using natural remedies or lifestyle changes?
Natural management strategies include wearing well-fitted supportive bras, maintaining a healthy weight, applying warm or cold compresses, gentle exercise, and reducing caffeine intake. Some women also find relief through stress reduction techniques and dietary modifications.
- When should I worry about breast pain after menopause, and what are the warning signs that I need to see a doctor?
Seek medical attention if you experience new, persistent pain in one area, pain accompanied by lumps or skin changes, nipple discharge, breast inflammation, or pain that significantly impacts daily activities. Any sudden or severe changes should be evaluated by a healthcare provider.
- Can hormone replacement therapy (HRT) for menopause symptoms increase the risk of experiencing breast pain?
Yes, HRT can sometimes cause or exacerbate breast pain. If you're experiencing breast pain while on HRT, your healthcare provider may need to adjust your dosage or consider alternative treatments.
- What are some differences between cyclic and noncyclic breast pain, and how does menopause affect these types of pain?
After menopause, breast pain is typically noncyclic, meaning it doesn't follow a regular pattern related to hormonal cycles. This differs from cyclic pain common before menopause, which often correlates with menstrual cycles. Postmenopausal breast pain is more likely to be localized and related to specific triggers or conditions.