Dealing with a yeast infection that won't go away can be incredibly frustrating and concerning. While most vaginal yeast infections respond well to over-the-counter treatments within a few days, some persist despite multiple treatment attempts or keep returning shortly after treatment ends. This persistent pattern affects millions of women and can significantly impact quality of life and intimate relationships.
Understanding why some yeast infections become stubborn or recurrent is crucial for finding effective solutions. Several underlying factors can contribute to treatment resistance, from incomplete treatment courses to more complex medical conditions that create an environment where yeast thrives. Recognizing when professional medical intervention is necessary can make the difference between ongoing frustration and successful resolution.
Understanding Treatment-Resistant Yeast Infections
A yeast infection that won't go away typically falls into one of two categories: persistent infections that don't respond to initial treatment, or recurrent infections that return within a few months. Persistent infections may continue showing symptoms even after completing a full course of antifungal medication, while recurrent infections seem to clear up temporarily before returning with similar intensity.
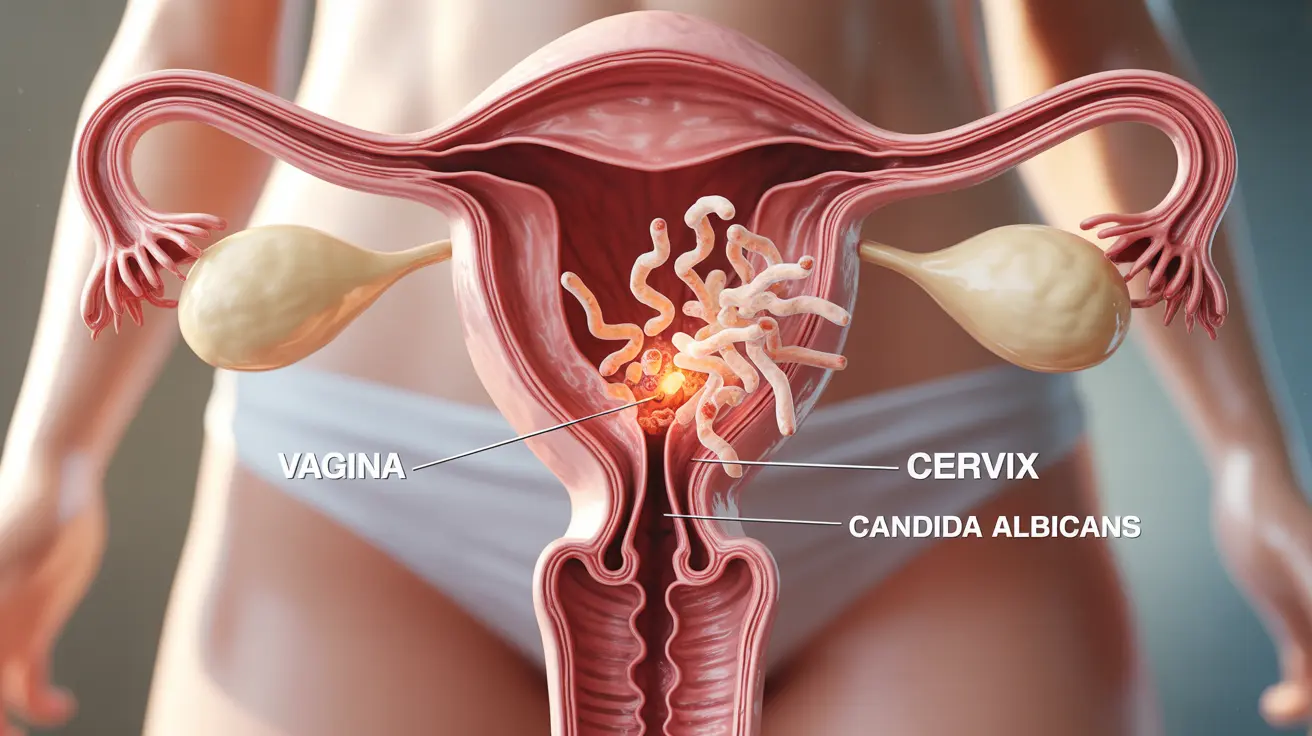
The most common culprit behind vaginal yeast infections is Candida albicans, a fungus that naturally exists in small amounts in the vaginal environment. However, when this balance is disrupted, Candida can multiply rapidly, leading to the uncomfortable symptoms of itching, burning, and thick white discharge that characterize yeast infections.
Sometimes, what appears to be a treatment-resistant yeast infection may actually be caused by a different species of Candida, such as Candida glabrata or Candida tropicalis, which can be more resistant to standard antifungal treatments. Additionally, other conditions like bacterial vaginosis or sexually transmitted infections can mimic yeast infection symptoms, leading to ineffective treatment attempts.
Common Causes of Persistent Yeast Infections
Several factors can contribute to yeast infections that resist treatment or keep returning. Antibiotic use is one of the most significant culprits, as these medications can disrupt the natural balance of bacteria in the vagina that normally keep yeast levels in check. Even a single course of antibiotics can trigger a yeast infection in susceptible individuals.
Hormonal fluctuations play a major role in yeast infection recurrence. Women often notice patterns related to their menstrual cycles, with infections occurring more frequently before menstruation when estrogen levels are higher. Pregnancy, birth control pills, and hormone replacement therapy can all create hormonal environments that encourage yeast overgrowth.
Diabetes and other conditions that affect blood sugar levels can make yeast infections more likely to persist. High glucose levels in blood and urine create an ideal environment for yeast to flourish. Even pre-diabetic conditions or poorly controlled diabetes can contribute to chronic yeast infection problems.
Compromised immune systems, whether due to stress, illness, medications, or conditions like HIV, can reduce the body's ability to control yeast populations naturally. Additionally, lifestyle factors such as wearing tight-fitting clothing, staying in wet bathing suits, using scented feminine products, or douching can create conditions that promote yeast growth and interfere with treatment effectiveness.
When to Seek Medical Attention
While over-the-counter treatments work for many yeast infections, certain situations warrant professional medical evaluation. If you've tried an over-the-counter antifungal medication for the full recommended duration without improvement, it's time to see a healthcare provider for proper diagnosis and stronger treatment options.
Recurrent infections—defined as four or more episodes within a year—require medical attention to identify underlying causes and develop a comprehensive treatment plan. Your doctor can perform tests to confirm the diagnosis, identify the specific type of yeast involved, and check for conditions that might be contributing to the problem.
Seek immediate medical care if you experience severe symptoms such as extensive swelling, painful urination, fever, or if you're pregnant. These symptoms could indicate a more serious infection or complications that require prompt treatment.
Additionally, if you have diabetes, are immunocompromised, or take medications that suppress your immune system, professional medical guidance is essential for managing yeast infections effectively and safely.
Prevention Strategies for Recurrent Infections
Preventing future yeast infections often requires a multi-faceted approach that addresses lifestyle factors and underlying health conditions. Maintaining good vaginal hygiene without overdoing it is crucial—this means gentle cleansing with warm water and avoiding harsh soaps, douches, or scented products that can disrupt the natural vaginal environment.
Clothing choices can significantly impact yeast infection risk. Wearing breathable, cotton underwear and avoiding tight-fitting pants or synthetic materials helps maintain proper airflow and moisture control. Changing out of wet clothing, especially bathing suits or workout gear, as soon as possible prevents creating the moist environment where yeast thrives.
Dietary modifications may help some women reduce their risk of recurrent infections. Limiting sugar and refined carbohydrates can help control yeast growth, while incorporating probiotics through yogurt or supplements may help maintain healthy vaginal flora. However, the evidence for dietary changes is mixed, and individual responses vary.
For women who experience yeast infections related to antibiotic use, discussing preventive antifungal treatment with a healthcare provider before starting antibiotics can be an effective strategy. Additionally, managing underlying health conditions like diabetes through proper blood sugar control is essential for preventing recurrent infections.
Advanced Treatment Options
When standard over-the-counter treatments fail, healthcare providers have several prescription options available. Longer courses of antifungal medications, typically lasting 7-14 days instead of the standard 1-3 days, may be necessary for stubborn infections. Prescription-strength topical medications or oral antifungals like fluconazole can provide more potent treatment.
For recurrent infections, maintenance therapy might be recommended. This typically involves taking an antifungal medication weekly or monthly for several months to prevent new infections from developing. The specific regimen depends on individual circumstances and the frequency of recurrence.
In cases where standard Candida albicans treatments aren't effective, laboratory testing can identify the specific yeast strain involved. Non-albicans Candida species may require different antifungal medications, such as boric acid suppositories or alternative oral antifungals.
Some healthcare providers may recommend combination approaches that include prescription medications along with lifestyle modifications and probiotic supplements to restore and maintain healthy vaginal flora. These comprehensive treatment plans address both the immediate infection and the underlying factors that contribute to recurrence.
Frequently Asked Questions
Why does my yeast infection keep coming back and won't go away?
Recurrent yeast infections can result from several factors, including incomplete treatment of the initial infection, underlying health conditions like diabetes or immune system disorders, hormonal fluctuations, frequent antibiotic use, or lifestyle factors that promote yeast growth. Sometimes, the infection is caused by a non-albicans Candida species that's more resistant to standard treatments. Identifying and addressing these underlying causes is key to breaking the cycle of recurrent infections.
What are the common causes of a yeast infection that won't respond to treatment?
Treatment-resistant yeast infections often occur when the infection is caused by a yeast strain other than Candida albicans, such as Candida glabrata, which may not respond to standard antifungal treatments. Other causes include using the medication incorrectly, not completing the full treatment course, having an undiagnosed underlying condition like diabetes, or the infection actually being something else entirely, such as bacterial vaginosis or a sexually transmitted infection that mimics yeast infection symptoms.
When should I see a doctor for a yeast infection that won't go away?
You should consult a healthcare provider if your symptoms persist after completing a full course of over-the-counter treatment, if you experience four or more yeast infections within a year, or if you have severe symptoms like extensive swelling, fever, or painful urination. Additionally, seek medical attention if you're pregnant, have diabetes, are immunocompromised, or if this is your first suspected yeast infection, as proper diagnosis is important to rule out other conditions.
How can I prevent recurrent or persistent yeast infections from returning?
Prevention strategies include wearing breathable cotton underwear, avoiding tight-fitting clothing, changing out of wet clothes promptly, and maintaining good hygiene without using harsh soaps or douches. Managing underlying health conditions like diabetes, discussing preventive antifungal treatment before taking antibiotics, and considering probiotic supplements may also help. Some women benefit from dietary changes, such as reducing sugar intake, though evidence for this approach varies.
What treatment options are available for drug-resistant or chronic yeast infections?
For persistent or recurrent infections, treatment options include longer courses of prescription antifungal medications, maintenance therapy with weekly or monthly antifungals, and alternative medications for non-albicans Candida species, such as boric acid suppositories. Your healthcare provider may order laboratory testing to identify the specific yeast strain and determine the most effective treatment. Comprehensive approaches that combine prescription medications with lifestyle modifications and probiotics are often most successful for chronic cases.