Breast reduction surgery, medically known as reduction mammoplasty, is a common procedure that helps women reduce physical discomfort and improve their quality of life. However, many women who undergo this surgery later wonder about their ability to breastfeed their children. The relationship between breast reduction and breastfeeding is complex, and the outcome varies significantly from person to person.
Understanding the factors that influence breastfeeding success after breast reduction surgery is crucial for women planning their families. While some women experience no difficulties with breastfeeding post-surgery, others may face challenges that require additional support and alternative feeding strategies.
Understanding Breast Reduction Surgery and Its Impact on Breastfeeding
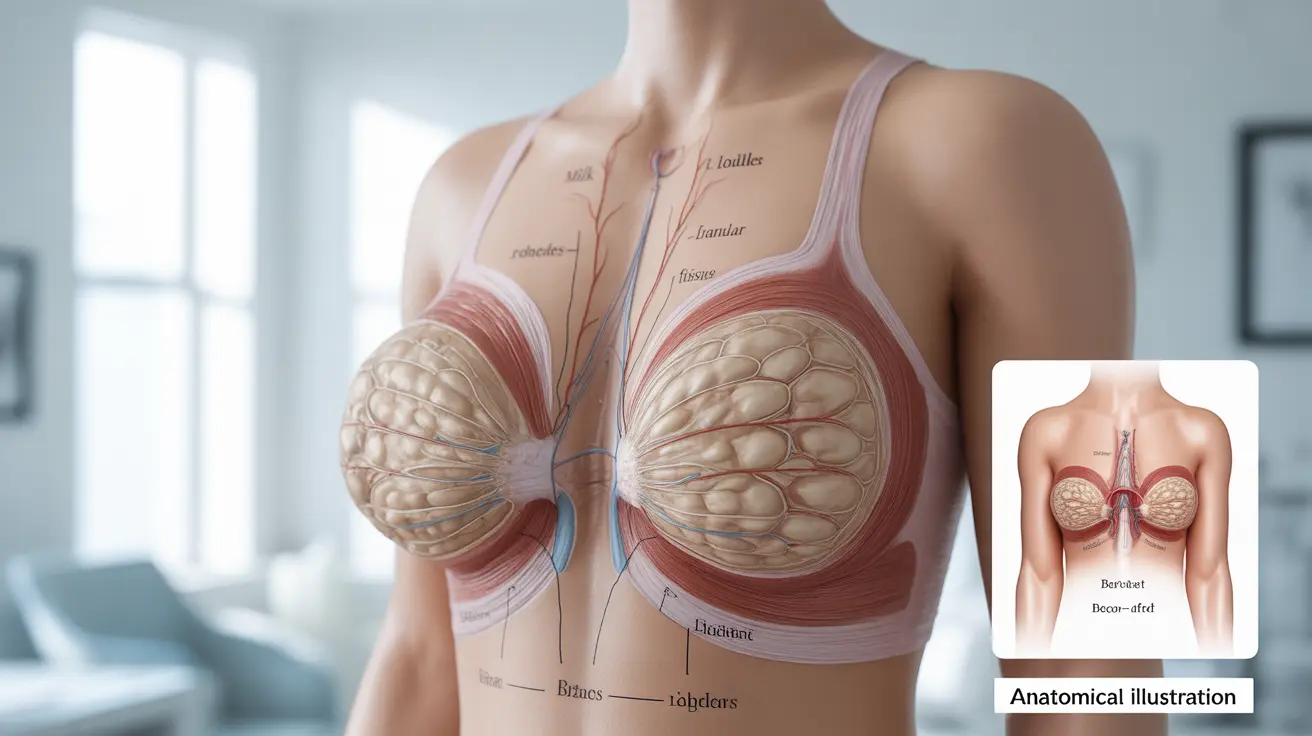
Breast reduction surgery involves removing excess breast tissue, fat, and skin to achieve a more proportionate breast size. During this procedure, surgeons may need to reposition the nipple and areola, which can potentially affect the milk ducts and nerves essential for successful breastfeeding.
The extent of surgical impact on breastfeeding depends largely on the specific technique used and how much breast tissue was removed. Some surgical approaches preserve more of the natural breast anatomy, while others may inadvertently damage the structures necessary for milk production and delivery.
It's important to understand that breast milk production relies on intact milk ducts that connect the milk-producing glands to the nipple. Additionally, proper nerve function is crucial for triggering the hormonal responses that initiate and maintain milk production.
Key Factors That Influence Breastfeeding Success
Surgical Technique and Timing
The surgical method used during your breast reduction plays a significant role in determining your breastfeeding capacity. Techniques that preserve the connection between the milk ducts and the nipple tend to result in better breastfeeding outcomes. Modern surgical approaches often prioritize maintaining these connections when possible.
The amount of tissue removed also matters considerably. Women who had minimal tissue removal are more likely to maintain their breastfeeding ability compared to those who underwent extensive reduction procedures.
Time Between Surgery and Pregnancy
The interval between your breast reduction surgery and pregnancy can affect your breastfeeding success. Allowing adequate healing time before pregnancy may improve your chances, as the breast tissue can regenerate to some extent over time.
Some medical professionals suggest that waiting at least one to two years after surgery before attempting pregnancy may optimize breastfeeding potential, though this timeline can vary based on individual healing processes.
Individual Healing and Anatomy
Every woman's body heals differently after breast reduction surgery. Some women experience better nerve regeneration and tissue recovery, which can positively impact their ability to produce and deliver breast milk.
Pre-existing factors such as breast anatomy, hormonal balance, and overall health also contribute to breastfeeding success rates after reduction surgery.
Strategies to Maximize Breastfeeding Success
Pre-Planning and Communication
If you're considering breast reduction surgery and plan to have children in the future, discuss your breastfeeding goals with your plastic surgeon beforehand. Many surgeons can modify their approach to better preserve breastfeeding function when they're aware of your future plans.
Document your surgical details, including the technique used and the amount of tissue removed. This information will be valuable for your healthcare providers during pregnancy and breastfeeding.
Prenatal Preparation
During pregnancy, work closely with a lactation consultant who has experience with post-surgical breastfeeding challenges. They can help you develop a personalized feeding plan and prepare for potential obstacles.
Consider taking breastfeeding classes that specifically address challenges related to previous breast surgery. These classes can provide valuable techniques and realistic expectations.
Postpartum Support Strategies
Immediate skin-to-skin contact after delivery can help stimulate milk production, regardless of your surgical history. This practice encourages the natural hormonal responses that support breastfeeding.
Frequent nursing or pumping sessions can help establish and maintain whatever milk production capacity you have. Even if your supply is limited, any amount of breast milk provides valuable benefits to your baby.
Alternative and Supplemental Feeding Options
Combination Feeding Approaches
Many women who have had breast reduction surgery successfully use combination feeding methods, which involve both breastfeeding and formula supplementation. This approach allows you to provide some breast milk benefits while ensuring your baby receives adequate nutrition.
Supplemental nursing systems (SNS) can be particularly helpful in these situations. These devices allow you to provide additional nutrition while your baby continues to nurse at the breast, which helps maintain the breastfeeding relationship and may stimulate continued milk production.
Monitoring Baby's Growth and Development
Regular weight checks and pediatric appointments are especially important when breastfeeding after breast reduction surgery. Your healthcare provider can help ensure your baby is receiving adequate nutrition and gaining weight appropriately.
Signs of adequate milk intake include regular wet diapers, consistent weight gain, and your baby appearing satisfied after feeding sessions. If concerns arise, early intervention with supplementation can help address nutritional needs.
Emotional and Psychological Considerations
The breastfeeding experience after breast reduction surgery can bring mixed emotions. Some women feel disappointed if their milk supply is lower than expected, while others are pleasantly surprised by their success.
It's important to remember that successful motherhood isn't defined solely by breastfeeding ability. Whether you breastfeed exclusively, use combination feeding, or rely primarily on formula, you're providing love and nutrition for your child.
Seeking support from other mothers who have experienced similar situations can be incredibly valuable. Online communities and support groups specifically for women who have breastfed after breast surgery can provide encouragement and practical advice.
Working with Healthcare Professionals
Building a supportive healthcare team is essential for breastfeeding success after breast reduction. Your team should include your obstetrician, pediatrician, and ideally a certified lactation consultant with experience in post-surgical breastfeeding challenges.
Don't hesitate to advocate for yourself and seek multiple opinions if needed. Some healthcare providers may be more knowledgeable about breastfeeding after breast surgery than others.
Frequently Asked Questions
Can you breastfeed after having a breast reduction surgery?
Yes, many women can breastfeed after breast reduction surgery, though the extent of success varies. The ability to breastfeed depends on factors such as the surgical technique used, the amount of tissue removed, and how well the milk ducts and nerves were preserved during the procedure. While some women maintain full breastfeeding capacity, others may have reduced milk supply and need to supplement with formula.
What factors affect the ability to breastfeed after breast reduction?
Several key factors influence breastfeeding success after breast reduction surgery. The surgical technique and whether milk ducts were preserved during the procedure play crucial roles. The amount of breast tissue removed, the time elapsed between surgery and pregnancy, individual healing patterns, and nerve regeneration all impact breastfeeding capacity. Additionally, the skill and approach of your surgeon in preserving breastfeeding-related anatomy significantly affects outcomes.
How can I increase my chances of successful breastfeeding after breast reduction?
To maximize your breastfeeding success, discuss your future breastfeeding goals with your surgeon before the procedure. Work with an experienced lactation consultant during pregnancy to develop a feeding plan. After delivery, initiate frequent nursing sessions and skin-to-skin contact to stimulate milk production. Consider using breast pumps between feedings to encourage supply, and don't hesitate to seek professional lactation support early if challenges arise.
Is it possible to exclusively breastfeed after breast reduction surgery?
Exclusive breastfeeding after breast reduction surgery is possible but less common than combination feeding approaches. Success depends largely on how much functional breast tissue and intact milk ducts remain after surgery. Some women do achieve exclusive breastfeeding, while others find that combination feeding with both breast milk and formula works best for their situation. Regular monitoring of your baby's weight gain and growth helps determine if exclusive breastfeeding is meeting their nutritional needs.
What support and strategies help with breastfeeding after breast reduction?
Effective support strategies include working with lactation consultants experienced in post-surgical breastfeeding challenges, joining support groups for mothers with similar experiences, and maintaining regular communication with your healthcare team. Practical strategies include using supplemental nursing systems if needed, monitoring your baby's weight closely, considering combination feeding approaches, and being flexible with your feeding plan. Professional support, realistic expectations, and emotional encouragement from family and friends are all valuable components of successful breastfeeding after breast reduction surgery.