Cephalosporins represent one of the most widely prescribed classes of antibiotics in modern medicine, playing a crucial role in treating bacterial infections across various medical settings. These beta-lactam antibiotics have evolved through multiple generations, each offering unique advantages in combating different types of bacterial pathogens.
Understanding how cephalosporins work, their applications, and proper usage is essential for both healthcare providers and patients seeking effective treatment for bacterial infections while minimizing the risk of antibiotic resistance.
Understanding Cephalosporins and Their Mechanism
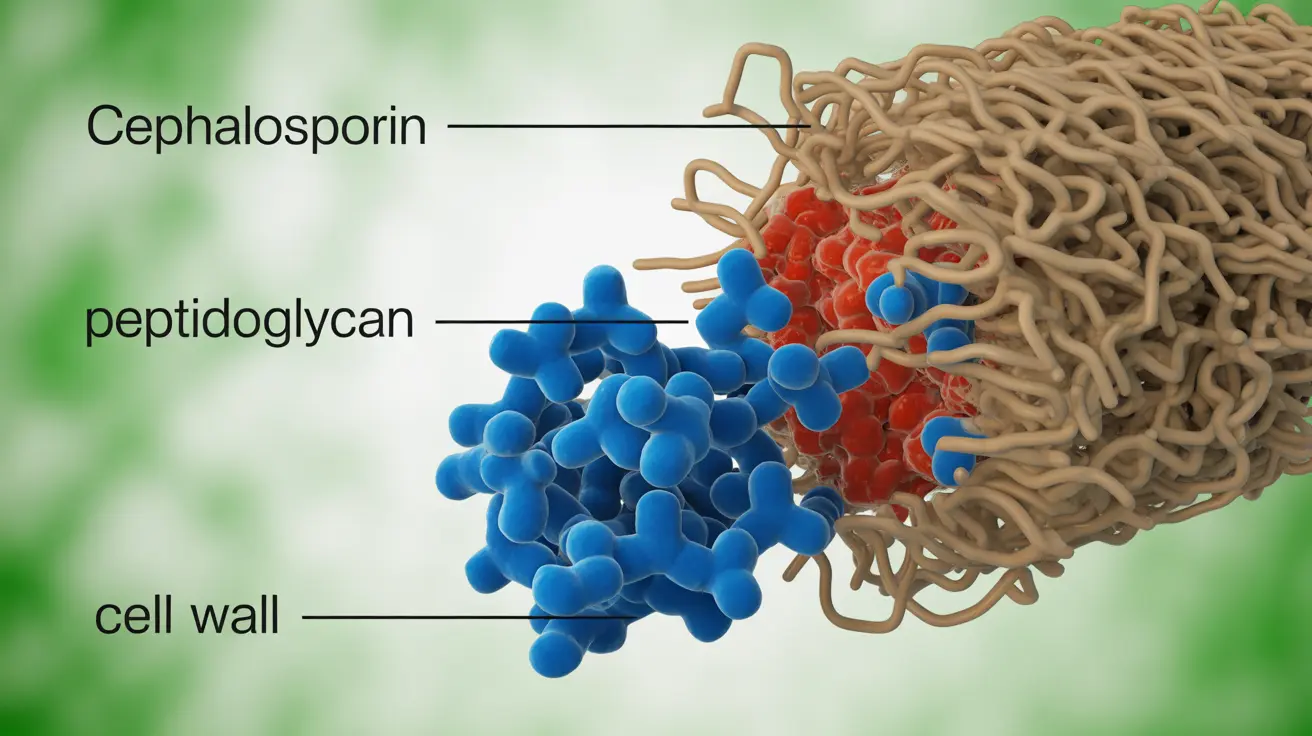
Cephalosporins belong to the beta-lactam family of antibiotics, sharing structural similarities with penicillin but offering broader spectrum activity against various bacteria. These medications work by disrupting bacterial cell wall synthesis, ultimately leading to bacterial cell death. The unique chemical structure of cephalosporins allows them to resist certain bacterial enzymes that would otherwise inactivate similar antibiotics.
The effectiveness of cephalosporins stems from their ability to bind to penicillin-binding proteins within bacterial cell walls, preventing the cross-linking necessary for cell wall stability. This mechanism makes them particularly effective against actively dividing bacteria, which is why timing and dosing schedules are critical for optimal treatment outcomes.
Generations of Cephalosporins: Spectrum and Applications
First-Generation Cephalosporins
First-generation cephalosporins, including cephalexin and cefazolin, primarily target gram-positive bacteria such as Staphylococcus and Streptococcus species. These medications are commonly prescribed for skin and soft tissue infections, urinary tract infections, and as prophylaxis before certain surgical procedures.
The limited spectrum of first-generation cephalosporins makes them ideal for targeted treatment when the causative organism is known to be susceptible, reducing the risk of disrupting beneficial bacterial flora unnecessarily.
Second-Generation Cephalosporins
Second-generation cephalosporins, such as cefuroxime and cefoxitin, offer expanded coverage against gram-negative bacteria while maintaining activity against many gram-positive organisms. This broader spectrum makes them valuable for treating respiratory tract infections, intra-abdominal infections, and certain types of pneumonia.
Some second-generation cephalosporins also demonstrate effectiveness against anaerobic bacteria, making them suitable for mixed infections where multiple bacterial types may be present.
Third-Generation Cephalosporins
Third-generation cephalosporins, including ceftriaxone and ceftazidime, provide excellent activity against gram-negative bacteria, including many strains resistant to earlier generations. These antibiotics are frequently used in hospital settings for serious infections such as meningitis, sepsis, and complicated urinary tract infections.
The enhanced penetration of third-generation cephalosporins into tissues and their ability to cross the blood-brain barrier makes them particularly valuable for treating central nervous system infections.
Fourth-Generation Cephalosporins
Fourth-generation cephalosporins, primarily represented by cefepime, offer broad-spectrum activity against both gram-positive and gram-negative bacteria, including some strains producing extended-spectrum beta-lactamases. These medications are typically reserved for serious nosocomial infections and multi-drug resistant bacterial infections.
Common Side Effects and Safety Considerations
Like all medications, cephalosporins can cause adverse reactions, though they are generally well-tolerated by most patients. Common side effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and abdominal cramping. These effects are usually mild and resolve after completing the antibiotic course.
More serious but rare side effects include allergic reactions, which can range from mild skin rashes to severe anaphylaxis. Clostridioides difficile-associated diarrhea represents another significant concern, particularly with prolonged or broad-spectrum cephalosporin use.
Certain cephalosporins may interact with alcohol, causing a disulfiram-like reaction characterized by flushing, nausea, and cardiovascular symptoms. Patients should be advised to avoid alcohol consumption during treatment and for several days after completion.
Cross-Reactivity with Penicillin Allergies
The relationship between penicillin allergies and cephalosporin safety has been extensively studied, revealing important nuances for clinical practice. While both antibiotics share the beta-lactam ring structure, the risk of cross-reactivity is lower than previously believed, particularly with newer generation cephalosporins.
Research indicates that patients with documented penicillin allergies have approximately a 1-3% risk of experiencing allergic reactions to cephalosporins, which is only slightly higher than the general population. The risk varies among different cephalosporin generations, with first-generation agents carrying slightly higher cross-reactivity potential.
Healthcare providers typically assess the severity and type of penicillin allergy before prescribing cephalosporins, with many patients safely receiving these antibiotics under appropriate medical supervision.
Preventing Antibiotic Resistance and Ensuring Effectiveness
Responsible use of cephalosporins is crucial for maintaining their effectiveness and preventing the development of antibiotic-resistant bacteria. Patients must complete the entire prescribed course, even if symptoms improve before finishing all doses. Stopping treatment prematurely can lead to incomplete bacterial eradication and potential resistance development.
Healthcare providers play a critical role in antibiotic stewardship by prescribing cephalosporins only when bacterial infections are suspected or confirmed, selecting the most appropriate generation based on the likely causative organism, and avoiding unnecessary broad-spectrum coverage when narrow-spectrum agents would suffice.
Regular monitoring of bacterial susceptibility patterns helps guide appropriate cephalosporin selection and dosing strategies, ensuring optimal treatment outcomes while minimizing resistance pressure on bacterial populations.
Frequently Asked Questions
What types of bacterial infections can cephalosporins effectively treat?
Cephalosporins are effective against a wide range of bacterial infections, including respiratory tract infections, urinary tract infections, skin and soft tissue infections, intra-abdominal infections, and certain types of meningitis. The specific infections treated depend on the generation of cephalosporin used, with each generation offering different spectrums of bacterial coverage. First-generation cephalosporins work well for gram-positive infections, while later generations provide broader coverage including gram-negative bacteria.
How do the different generations of cephalosporins compare in treating various bacteria?
Each generation of cephalosporins offers progressively broader bacterial coverage. First-generation agents primarily target gram-positive bacteria like Staphylococcus and Streptococcus. Second-generation cephalosporins expand coverage to include more gram-negative bacteria and some anaerobes. Third-generation agents provide excellent gram-negative coverage and can penetrate the central nervous system. Fourth-generation cephalosporins offer the broadest spectrum, including activity against some multi-drug resistant organisms while maintaining gram-positive coverage.
What are the common side effects and serious risks associated with cephalosporin antibiotics?
Common side effects of cephalosporins include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and stomach upset. More serious risks include allergic reactions ranging from mild rashes to severe anaphylaxis, Clostridioides difficile-associated diarrhea, and potential interactions with alcohol in certain cephalosporins. Some patients may experience injection site reactions with intravenous formulations. Most side effects are mild and resolve after completing treatment.
Can people with penicillin allergies safely take cephalosporins?
Many people with penicillin allergies can safely take cephalosporins, as the cross-reactivity risk is relatively low at approximately 1-3%. However, this decision should always be made by a healthcare provider who can assess the severity and type of penicillin allergy. Patients with severe penicillin allergies or anaphylactic reactions may require alternative antibiotics or careful monitoring if cephalosporins are prescribed. The risk varies slightly among different generations of cephalosporins.
How should cephalosporins be used to prevent antibiotic resistance and ensure effectiveness?
To prevent antibiotic resistance, patients must complete the entire prescribed course of cephalosporins, even if symptoms improve early. Healthcare providers should prescribe the most appropriate generation and narrowest spectrum necessary for the infection. Cephalosporins should only be used for confirmed or strongly suspected bacterial infections, not viral illnesses. Proper dosing and timing are essential, and patients should never share antibiotics or save leftover doses for future use. Regular monitoring of bacterial susceptibility patterns helps guide appropriate prescribing practices.