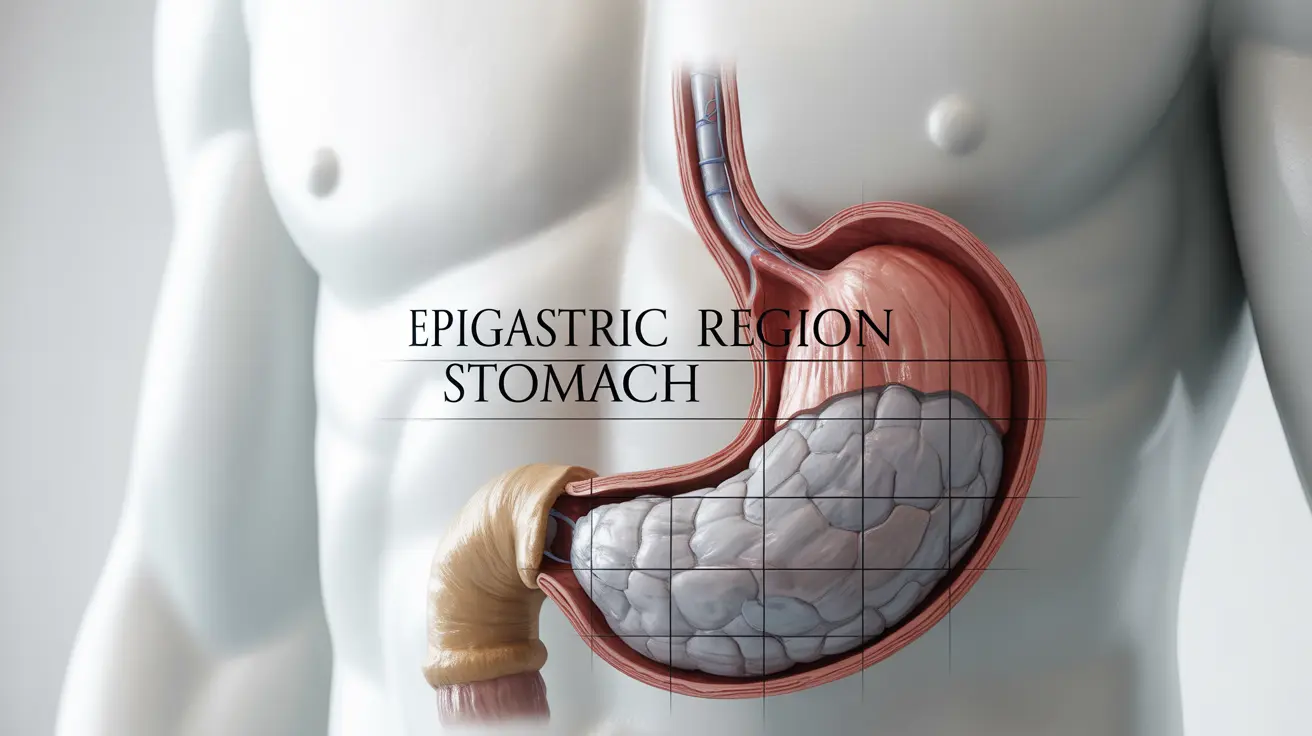
Epigastric pain, which occurs in the upper central region of the abdomen, can be a concerning symptom that affects many people. This discomfort, located just below the ribcage and above the navel, may range from mild to severe and can signal various underlying conditions requiring medical attention.
Understanding the nature of epigastric pain, its potential causes, and appropriate treatment options is crucial for managing this common health concern effectively. This comprehensive guide will help you recognize when to seek medical care and how to address your symptoms.
Common Causes of Epigastric Pain
Epigastric pain can stem from several different conditions affecting the digestive system and surrounding organs:
Gastroesophageal Reflux Disease (GERD)
GERD is a frequent cause of epigastric pain, characterized by acid reflux and heartburn. The pain typically worsens after meals or when lying down, and may be accompanied by a burning sensation in the chest.
Gastritis
Inflammation of the stomach lining can lead to sharp or burning epigastric pain. This condition may be acute or chronic and is often triggered by certain medications, excessive alcohol consumption, or bacterial infections.
Peptic Ulcers
These painful sores in the stomach or small intestine lining can cause persistent epigastric pain that may improve or worsen with eating.
Other Notable Causes
- Pancreatitis
- Gallbladder problems
- Hiatal hernia
- Gastric cancer (less common)
Diagnosis and Medical Assessment
Healthcare providers use various methods to diagnose the cause of epigastric pain:
Physical Examination
Doctors typically begin with a thorough physical examination and detailed medical history to understand the nature and pattern of your pain.
Diagnostic Tests
Common diagnostic procedures may include:
- Upper endoscopy
- Blood tests
- Imaging studies (CT scan, ultrasound)
- H. pylori testing
- pH monitoring
Treatment Approaches
Treatment for epigastric pain varies depending on the underlying cause:
Medication Options
- Antacids
- Proton pump inhibitors (PPIs)
- H2 blockers
- Antibiotics (if H. pylori is present)
Lifestyle Modifications
Several lifestyle changes can help manage and prevent epigastric pain:
- Maintaining a healthy diet
- Eating smaller, more frequent meals
- Avoiding trigger foods
- Staying upright after meals
- Stress management techniques
Warning Signs and Emergency Situations
Certain symptoms warrant immediate medical attention:
- Severe, persistent pain
- Difficulty breathing
- Chest pain or pressure
- Vomiting blood
- Black or tarry stools
- Unexplained weight loss
Frequently Asked Questions
What are the most common causes of epigastric pain and how can I identify them?
The most common causes include GERD, gastritis, and peptic ulcers. You can identify them through the timing and nature of pain, associated symptoms, and whether the pain improves or worsens with eating or specific activities.
How is epigastric pain diagnosed by doctors and what tests might be involved?
Doctors typically start with a physical examination and medical history, followed by diagnostic tests such as endoscopy, blood work, imaging studies, and H. pylori testing when necessary.
What treatments are effective for managing epigastric pain caused by acid reflux or gastritis?
Effective treatments include acid-reducing medications like PPIs or H2 blockers, lifestyle modifications, dietary changes, and treating any underlying conditions. Some patients benefit from probiotics and stress reduction techniques.
When should I seek urgent medical care for epigastric pain?
Seek immediate medical attention if you experience severe, persistent pain, difficulty breathing, chest pain, vomiting blood, black stools, or unexplained weight loss.
Can lifestyle or dietary changes help prevent or reduce epigastric pain symptoms?
Yes, lifestyle modifications such as eating smaller meals, avoiding trigger foods, maintaining a healthy weight, reducing alcohol intake, and managing stress can significantly help prevent and reduce epigastric pain symptoms.