Experiencing shortness of breath after recovering from COVID-19 can be concerning and frustrating for many individuals. This persistent symptom, also known as post-COVID dyspnea, affects numerous COVID-19 survivors and can significantly impact daily activities and quality of life.
Understanding the causes, duration, and available treatments for post-COVID breathing difficulties is crucial for proper management and recovery. This comprehensive guide explores what you need to know about dealing with shortness of breath after COVID-19 and when to seek professional help.
Understanding Post-COVID Shortness of Breath
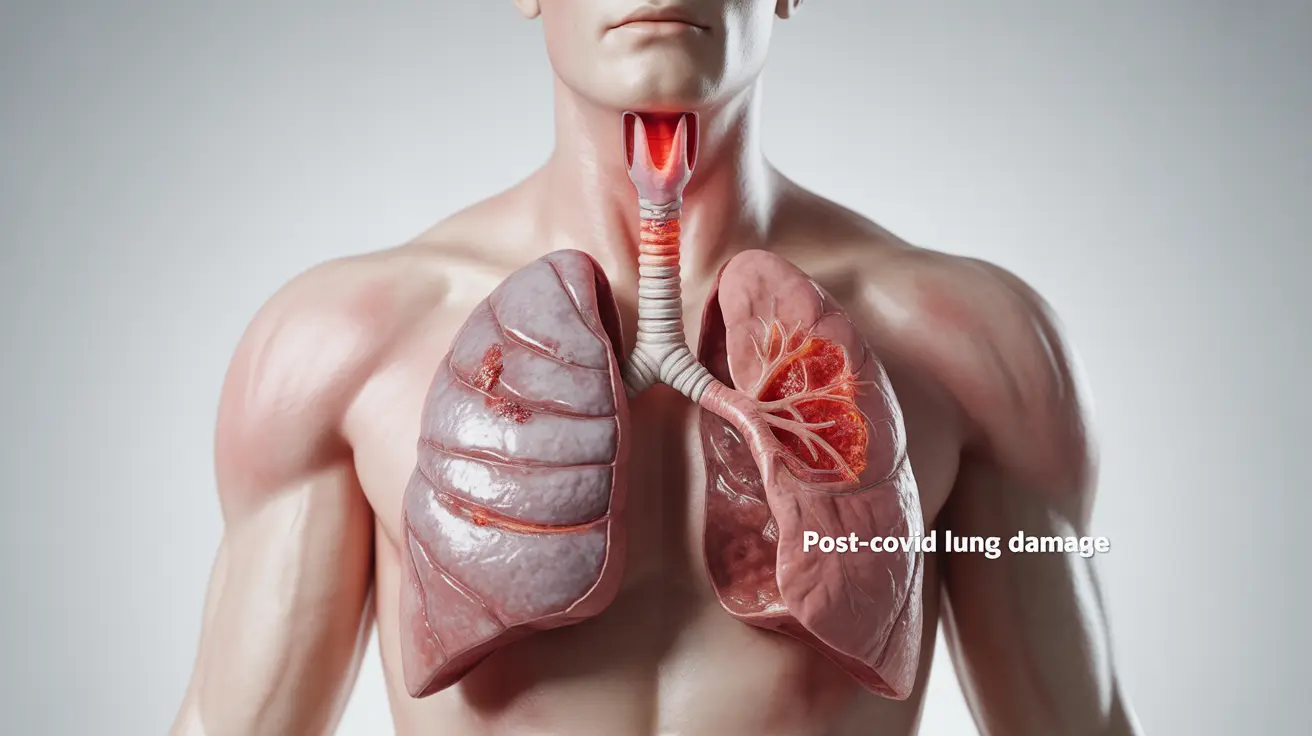
Post-COVID shortness of breath occurs due to several factors, including inflammation in the airways, damage to lung tissue, and reduced lung capacity following the infection. Some individuals may experience this symptom as part of long COVID syndrome, where symptoms persist well beyond the initial infection period.
Common Manifestations
Post-COVID breathlessness may present in various ways:
- Difficulty breathing during physical activities
- Feeling winded after minimal exertion
- Trouble taking deep breaths
- Chest tightness or discomfort
- Increased breathing rate during rest
Recovery Timeline and Expectations
The duration of post-COVID shortness of breath varies significantly among individuals. While some people may notice improvement within weeks, others might experience symptoms for several months. Recovery often depends on factors such as the severity of the initial infection, pre-existing conditions, and overall health status.
Treatment Approaches and Management Strategies
Medical Interventions
Healthcare providers may recommend various treatments to address post-COVID breathing difficulties:
- Inhaled medications to reduce airway inflammation
- Prescribed breathing exercises
- Pulmonary rehabilitation programs
- Supplemental oxygen therapy (in severe cases)
- Medications to manage underlying inflammation
Breathing Exercises and Rehabilitation
Specific breathing exercises can help improve lung function and reduce breathlessness:
- Pursed-lip breathing
- Diaphragmatic breathing
- Position-based breathing techniques
- Gradual aerobic exercise as tolerated
- Controlled coughing exercises
When to Seek Medical Attention
It's important to consult a healthcare provider if you experience:
- Worsening shortness of breath
- Difficulty breathing while at rest
- Chest pain or pressure
- Bluish lips or face
- Inability to speak in full sentences due to breathlessness
Frequently Asked Questions
What causes shortness of breath after recovering from COVID-19?
Shortness of breath after COVID-19 typically results from inflammation and potential damage to lung tissue during infection. The virus can affect the airways and air sacs in the lungs, leading to reduced lung function and breathing difficulties even after recovery from the acute infection.
How long can shortness of breath last after a COVID-19 infection?
The duration varies among individuals. Some people may experience improvement within 4-6 weeks, while others might have symptoms persisting for several months. Long COVID cases may experience breathlessness for 6 months or longer.
What treatments are available to manage persistent shortness of breath after COVID-19?
Treatment options include pulmonary rehabilitation, breathing exercises, medications to reduce inflammation, and supplemental oxygen when necessary. The specific treatment plan depends on the severity of symptoms and individual patient needs.
Can breathing exercises help improve lung function and reduce breathlessness after COVID-19?
Yes, breathing exercises can significantly improve lung function and reduce breathlessness. Techniques such as pursed-lip breathing, diaphragmatic breathing, and controlled breathing exercises, especially when part of a structured rehabilitation program, can help strengthen respiratory muscles and improve breathing efficiency.
When should I see a doctor if I continue to experience shortness of breath following COVID-19?
Seek medical attention if you experience worsening breathlessness, difficulty breathing at rest, chest pain, bluish discoloration of lips or face, or if breathlessness significantly impacts your daily activities. Immediate medical care is necessary if you develop severe breathing difficulties or chest pain.