An orchiectomy is a surgical procedure that involves the removal of one or both testicles. This important medical intervention serves various purposes, from treating testicular cancer to supporting gender-affirming care. Understanding what an orchiectomy entails, its different types, and potential impacts can help patients make informed decisions about their healthcare journey.
Whether recommended for medical necessity or chosen as part of gender transition, this procedure requires careful consideration of its effects on hormonal balance, fertility, and overall health. Let's explore the essential aspects of orchiectomy, including its purposes, procedures, and recovery process.
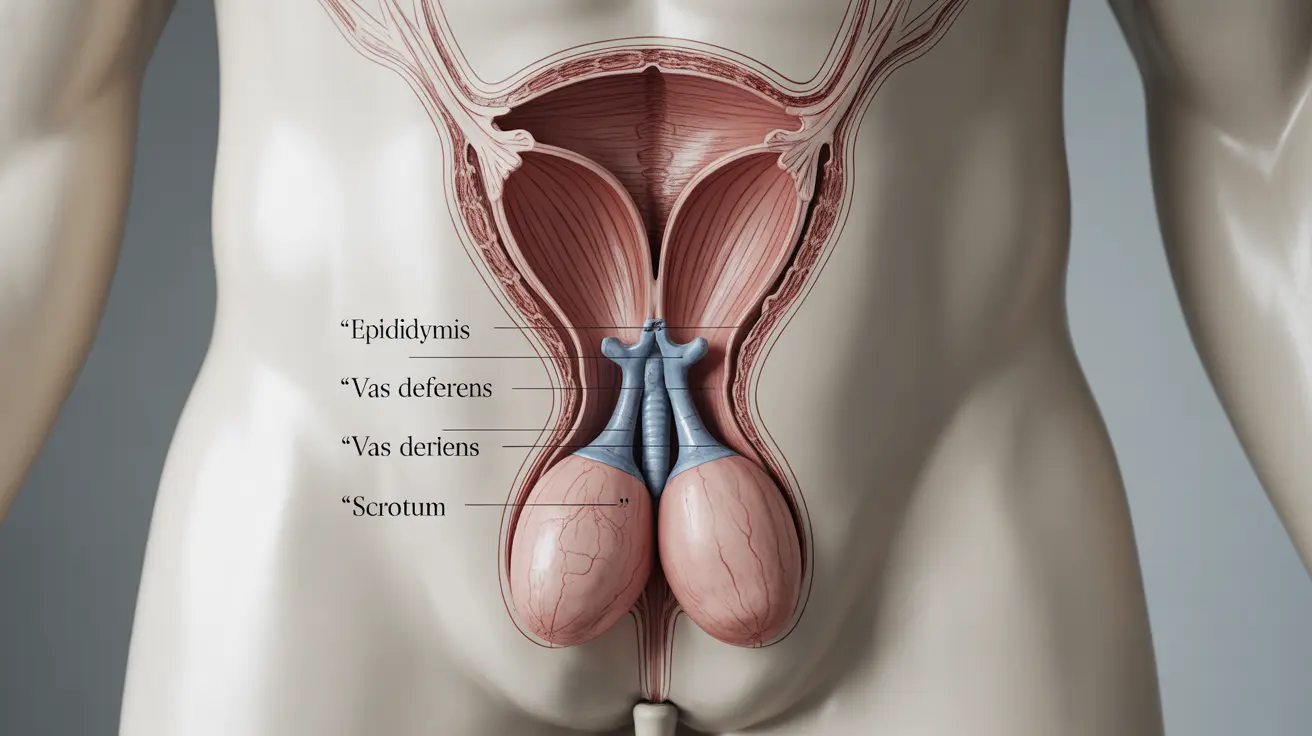
Types of Orchiectomy Procedures
There are several types of orchiectomy procedures, each serving specific medical needs:
Radical Orchiectomy
This procedure involves removing the entire testicle and spermatic cord through an incision in the groin area. It's typically performed to treat testicular cancer and ensures the complete removal of potentially cancerous tissue.
Simple Orchiectomy
A simple orchiectomy removes only the testicle(s), leaving the scrotum intact. This type is often chosen for hormone therapy in prostate cancer treatment or as part of gender-affirming surgery.
Bilateral Orchiectomy
When both testicles are removed, it's called a bilateral orchiectomy. This may be necessary for advanced prostate cancer treatment or chosen for gender transition purposes.
Medical Reasons for Orchiectomy
Orchiectomy procedures are performed for various medical conditions:
- Testicular cancer treatment
- Advanced prostate cancer management
- Severe testicular trauma
- Gender-affirming care
- Chronic testicular pain
- Treatment of testicular torsion complications
Impacts on Hormone Levels and Fertility
An orchiectomy significantly affects the body's hormone production and reproductive capabilities. The testicles produce approximately 95% of the body's testosterone, so their removal leads to a dramatic decrease in testosterone levels. This can result in various physical changes, including:
- Decreased muscle mass
- Reduced body hair growth
- Changes in fat distribution
- Possible mood changes
- Loss of fertility
- Reduced libido
Recovery and Post-Surgery Care
Recovery from an orchiectomy typically involves:
- Initial rest period of 24-48 hours
- Limited physical activity for 1-2 weeks
- Pain management with prescribed medications
- Regular wound care and monitoring
- Follow-up appointments with healthcare providers
- Hormone replacement therapy if prescribed
Long-term Considerations
After an orchiectomy, patients should consider several long-term factors:
- Regular medical check-ups
- Monitoring hormone levels
- Bone density screenings
- Emotional and psychological support
- Lifestyle adjustments
- Possible prosthetic options
Frequently Asked Questions
What is an orchiectomy and why is it performed? An orchiectomy is a surgical procedure to remove one or both testicles. It's performed to treat testicular cancer, manage advanced prostate cancer, provide gender-affirming care, or address severe testicular trauma or pain.
How does orchiectomy affect testosterone levels and fertility? An orchiectomy significantly reduces testosterone production and eliminates fertility in the affected testicle(s). This leads to decreased muscle mass, changes in body composition, and the inability to produce sperm in the removed testicle(s).
What are the different types of orchiectomy surgeries and their purposes? The main types include radical orchiectomy (removing testicle and spermatic cord), simple orchiectomy (removing only the testicle), and bilateral orchiectomy (removing both testicles). Each type serves specific medical purposes ranging from cancer treatment to hormone therapy.
What should I expect during recovery and what are the risks after an orchiectomy? Recovery typically takes 1-2 weeks of limited activity. Risks include infection, bleeding, chronic pain, and hormonal changes. Most patients can return to normal activities within a few weeks with proper care.
Are there alternatives to orchiectomy for reducing testosterone in prostate cancer treatment? Yes, alternatives include hormone therapy medications (LHRH agonists or antagonists), anti-androgens, and other pharmaceutical approaches. However, orchiectomy might be recommended in specific cases for its permanent and cost-effective nature.